Mixed Adenoma-Serrated Polyp
Alexandros D. Polydorides, MD, PhD
Key Facts
Etiology/Pathogenesis
Serrated path: HP → SSA/P → MASP → TSA → cancer?
MSI, CIMP (MGMT, hMLH1), BRAF mutations
Clinical Issues
0.5% of polyps; right-sided, pedunculated, > 0.5 cm
Complete removal (polypectomy), as with adenomas
Microscopic Pathology
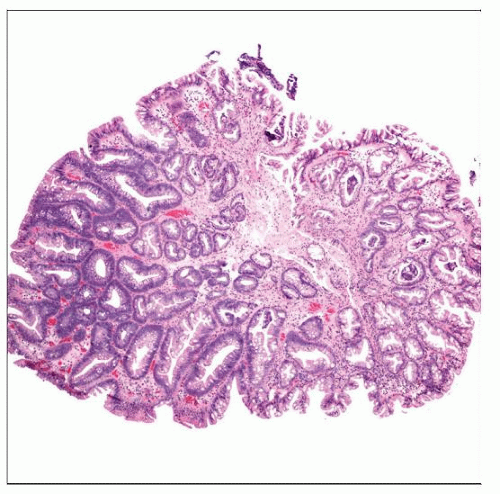
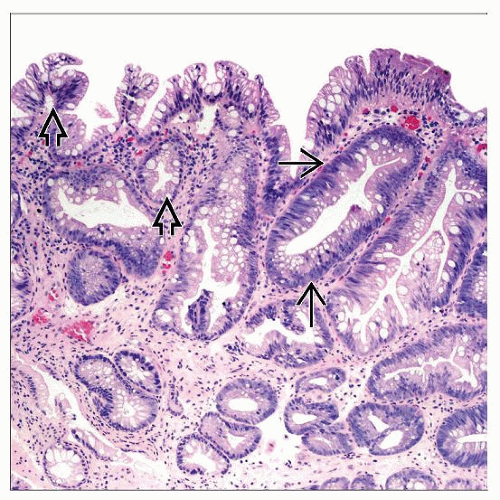
2 distinct, adjacent, or intermingled components
HP: Basal small nuclei, hypermucinous cytoplasm
Adenoma: Crowded tubules, large stratified nuclei
Pronounced serration: Often throughout lesion
Top Differential Diagnoses
(Traditional) serrated adenoma
Dysplastic epithelium throughout lesion
Infolding, nuclear budding, and papillary tufting
Hypereosinophilic cytoplasm, prominent nucleoli
Lack of surface maturation, immature goblet cells
TERMINOLOGY
Abbreviations
Mixed adenoma-serrated polyp (MASP)
(Traditional) serrated adenoma (TSA)
Hyperplastic polyp (HP)
Sessile serrated adenoma/polyp (SSA/P)
Synonyms
Mixed hyperplastic adenomatous polyp (MHAP), mixed (admixed) polyp, mixed TSA-SSA/P
Definitions
Polyp with discrete (adjacent or admixed) areas of adenoma (overt dysplasia) and HP (serrated lumens)
Most MASP are combinations of HP (or SSA/P) and TSA
Adenomatous component also has serrated contour
TSA occurs on its own (not part of mixed polyp)
Serrated polyps = HP, MASP, SSA/P, and TSA
ETIOLOGY/PATHOGENESIS
Theories of Pathogenesis
Coincidental colocalization of 2 separate polyps
Unlikely: Histologically admixed, occur often
Hyperplastic areas originate from adenomatous areas
Differentiation, maturation process
HP induced to grow by adjoining adenoma
Single pathway of pathogenesis
More differentiated original epithelial cell
Adenomatous transformation of HP
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree