Miscellaneous HIV-associated Renal Diseases
A. Brad Farris, III, MD
TERMINOLOGY
Abbreviations
HIV-associated renal diseases (HIV-ARD)
Definitions
Renal diseases other than collapsing glomerulopathy (HIVAN) that occur particularly in patients infected with HIV, due to direct effect on kidney, altered immune system, or drug toxicity
HIV-ASSOCIATED LUPUS-LIKE GLOMERULONEPHRITIS
Terminology
Chronic immune complex disease in HIV-infected patients that has LM, IF, and EM features of lupus nephritis, but patients have no other evidence of lupus nephritis
Described by Haas et al and Nochy et al
Pathogenesis
Probably related to immune dysregulation
Loss of CD4(+) T regulatory cells causes autoimmune disease
Role of infectious agent not excluded
Incidence
Possibly 2nd most common form of glomerular lesions (after HIVAN) in HIV patients undergoing biopsy
Many (13/14 in the Haas Baltimore study) were African-American
Nochy’s study in Europe showed equal proportions of whites and blacks having lupus-like GN
In series of > 100 biopsies for glomerular disease in HIV(+) patients, 3% had lupus-like GN
Presentation
Hematuria and proteinuria/nephrotic syndrome
Share other features such as anemia, leukopenia, multiorgan involvement, and serositis
Laboratory Tests
± ANA and anti-double-stranded (ds) DNA and ↓ complements
Assessment somewhat complicated because some HIV patients have low-titer ANAs
Screening of > 150 patients with AIDS found 19 to be ANA(+) but only 2 at high titer and none anti-dsDNA Ab(+)
Treatment
Corticosteroids, ACE inhibitors, highly active antiretroviral therapy (HAART) have all been used
Prognosis
Outcome can be poor, because many patients present with advanced disease
Microscopic Pathology
Focal/diffuse proliferative GN or membranous nephropathy
Immunofluorescence
“Full house” pattern of IgG, IgA, IgM, C3, and C1q
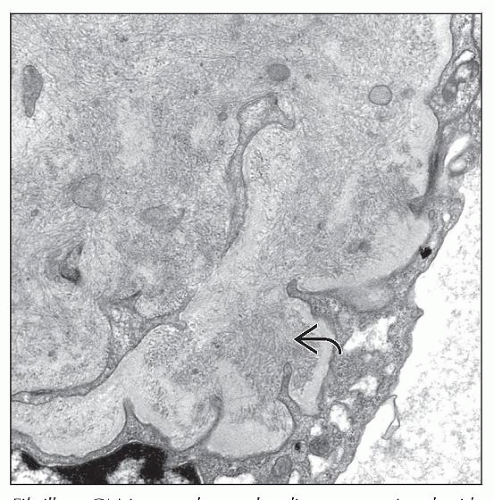
Electron Microscopy
Essentially all have tubuloreticular inclusions
Most common pattern appears to be combination of mesangial, subendothelial, subepithelial, and intramembranous deposits
Differential Diagnosis
IgA NEPHROPATHY
Terminology
IgA(+) glomerular disease arising in HIV(+) patients that has clinical and pathologic aspects similar to idiopathic IgA nephropathy
Reports have also included Henoch-Schönlein purpura with nephritis
Pathogenesis
Deposits eluted from glomeruli have shown specificity for HIV envelope (e.g., gp41, gp120, gp160) or core proteins (e.g., p24) (Kimmel et al)
Incidence
Series (many of which are from Europe) indicate higher incidence of IgA nephropathy in white patients with HIV infection
Data conflicts regarding prevalence of IgA deposits in patients dying from AIDS
Some series indicate high prevalence of IgA deposits in AIDS patients, but this does not necessarily correlate with increased IgA nephropathy rate
Presentation
Hematuria and low-grade proteinuria are common
May present with Henoch-Schönlein purpura (HSP)-type picture (rash [leukocytoclastic angiitis of the skin], etc.)
Laboratory Tests
Associated with IgA-containing cryoglobulins
↑ IgA levels, IgA-containing circulating immune complexes, and IgA-rheumatoid factor
Treatment
ACE inhibitors may be useful
Prognosis
Thought to be same as IgA nephropathy in non-HIV-infected patients
Microscopic Pathology
Does not differ drastically from conventional IgA nephropathy seen in absence of HIV
Mesangial proliferation ± collapsing glomerulosclerosis (coexisting HIVAN)
Immunofluorescence
Shows mesangial IgA deposits like conventional IgA nephropathy seen in absence of HIV
Electron Microscopy
In contrast with idiopathic IgA nephropathy, there are also numerous tubuloreticular structures that provide a clue to presence of HIV
THROMBOTIC MICROANGIOPATHY (TMA)
Terminology
TMA associated with HIV infection
Both syndromes resembling thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) can occur in HIV-infected patients
Pathogenesis
Etiology not known
HIV injury to endothelium or infection of megakaryocytes may be involved
Escherichia coli 0157:H7 appears not to be involved
Appears that ADAMTS13 level is not ↓ in HIV-associated TMA as it is in TTP
Etiology role has been attributed to CMV infection, cryptosporidiosis, AIDS-related neoplasia, drugs, and antiphospholipid antibodies
Incidence
Human data are lacking
Multicenter autopsy study showed 15 of 214 patients (7%) with deaths attributable to AIDS had evidence of TMA
French study (Peraldi et al) attributed rapid decline in renal function to HUS-type syndrome in 32 of 92 patients
6/27 (22.2%) pigtailed macaques (Macaca nemestrina) acutely infected with HIV-2 developed histological and EM features of renal TMA such as glomerular capillary platelet thrombi and mesangiolysis
Presentation
Acute renal failure ± proteinuria and hematuria
Microangiopathic hemolytic anemia and thrombocytopenia
Presentations may be classified as either HUS or TTP (neurologic symptoms and fever)
Laboratory Tests
± thrombocytopenia ± schistocytosis
Treatment
Treatment of underlying HIV may be best approach
Plasmapheresis and fresh frozen plasma have been used
Rituximab and corticosteroids have been used
Hemodialysis may be needed at presentation
Prognosis
High mortality: More severe in HIV-infected patients than in non-HIV-infected patients
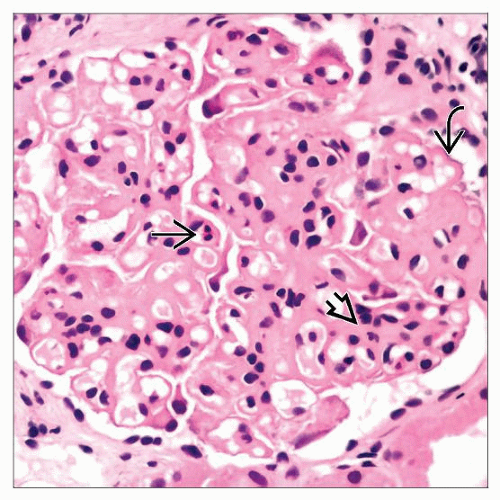
Microscopic Pathology
Pathologic findings are similar to those of TMA in non-HIV-infected patients
Mucoid arterial intimal hyperplasia and intraluminal thrombi may be observed
Fragmented intramural RBCs in vessels
May coexist with HIVAN