Minimal Change Disease
A. Brad Farris, III, MD
Key Facts
Terminology
Synonyms: Lipoid nephrosis, nil disease
Etiology/Pathogenesis
Usually idiopathic
Involves loss of glomerular negative charge
Circulating permeability factor
Secondary forms due to virus, drugs, lymphoma
Clinical Issues
Nephrotic syndrome
Most common in young children, boys > girls
90-95% respond to corticosteroids
Can present as acute renal insufficiency in adults
Microscopic Pathology
Glomerulus normal by light microscopy except for variable podocyte hypertrophy
Resorption droplets in tubules
Ancillary Tests
IF negative except for variable focal IgM ± C3
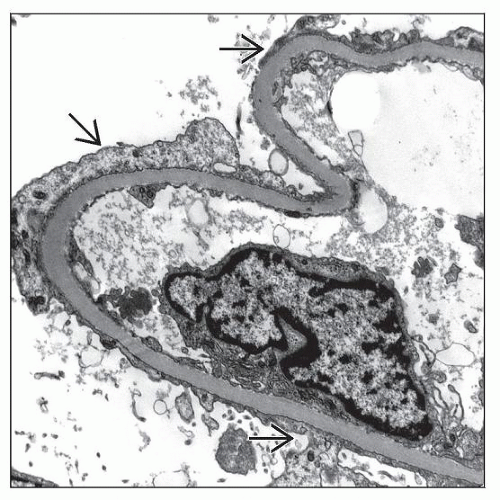
EM shows podocyte foot process effacement, normal GBM, and no deposits
Top Differential Diagnoses
Focal segmental glomerulosclerosis (FSGS)
Diffuse mesangial hypercellularity (DMH)
IgA, IgM, or C1q nephropathy
Diagnostic Checklist
Examination of biopsy at multiple levels may prevent missed diagnosis of FSGS
Note whether biopsy includes corticomedullary junction, the site initially affected by FSGS
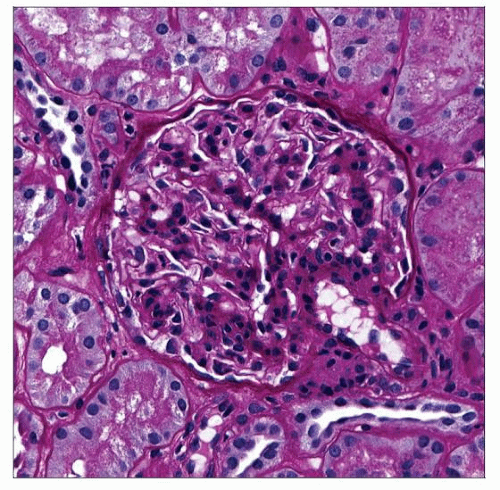 A biopsy with minimal change disease shows a normal glomerulus on PAS stain without GBM thickening or inflammatory cells and with minimal mesangial hypercellularity. |
TERMINOLOGY
Abbreviations
Minimal change disease (MCD)
Synonyms
Lipoid nephrosis
Nil disease
Minimal change nephrotic syndrome
Minimal change glomerulopathy
Definitions
Idiopathic glomerular disease that causes nephrotic syndrome, with little or no light or immunofluorescent microscopic abnormalities and podocyte foot process effacement on electron microscopy
Occurs as primary (idiopathic) disease, especially in children, and secondary to drugs, allergic reactions, and neoplasia at all ages
ETIOLOGY/PATHOGENESIS
Idiopathic (Primary)
Classified as disease of podocytes, a “podocytopathy”
Loss of podocyte negatively charged glycocalyx a central feature
Cause unknown; possibilities include
Enzymatic cleavage (e.g., neuraminidase)
Neutralizing positively charged molecule
Decreased synthesis
Loss of negative (anionic) charge leads to
Selective leakage of albumin
Albumin is most negatively charged of major plasma proteins
Foot process effacement
Circulating permeability factor or cytokine abnormality postulated
Various substances have been suggested, ranging in molecular weight from 12-160 kDa
IL-13, an anti-inflammatory Th2 cytokine for B cells and monocytes, is implicated
T-cell IL-13 content increases during relapse
Increased serum IgE, IgG4 in some patients
Secondary Forms of MCD
Infection
Human immunodeficiency virus (HIV)
Upper respiratory tract infection
Hodgkin disease and other lymphoproliferative disorders (lymphoma)
Possibly related to abnormal T-cell function
Allergy
Drugs, especially nonsteroidal anti-inflammatory drugs
Bee venom
Immunization
Mononucleosis
Systemic lupus erythematosus
Graft vs. host disease
Acute renal allograft rejection (rare manifestation)
Experimental Studies
Key features of MCD (e.g., foot process effacement [FPE], proteinuria) reproduced in rats or mice by
Overexpression of IL-13
Administration of puromycin aminonucleoside or Adriamycin
Supernatants from hybridomas made from T cells from patients with MCD
Administration of neuraminidase or protamine sulfate (removes sialic acid or neutralizes anionic charge, respectively)
CLINICAL ISSUES
Epidemiology
Age
Most common in children (65-75% of cases)
Median age of onset is 2.5 years
Peak incidence is at 2-3 years
Causes ˜ 90% of nephrotic syndrome in preadolescents and ˜ 50% in adolescents
Adults have late peak incidence, > 80 years old
26% of adults with nephrotic syndrome are < 65 years
20% are 65-79 years
46% are 80-91 years
Gender
In children, 2:1 ratio of males to females
In adults: Equal gender distribution
Ethnicity
More common in whites and Asians than in blacks
Presentation
Sudden (days) onset of nephrotic syndrome
Nephrotic syndrome
Proteinuria defined as ≥ 3.5 g/d in adults and ≥ 40 mg/m2 body surface area (BSA)/hr in timed overnight collection in children
Selective proteinuria (chiefly albumin)
Edema
Hypoalbuminemia defined as serum albumin < 3.5 g/dL in adults and < 2.5 g/dL in children
Hypercholesterolemia
Lipiduria
Lipid-laden enucleated tubular cells may be seen as “oval fat bodies” in urinary sediment, with polarizable lipid
Gave rise to the term “lipoid nephrosis,” original term for MCD
Hematuria
Microscopic hematuria (10-30% of cases)
Renal dysfunction
Acute renal insufficiency may occur in adults with MCD from acute ischemic tubular injury due to poor perfusion
Associated with extreme hypoalbuminemia
May be accompanied by anasarca
Most recover with steroids and diuretics
Renal insufficiency (plasma creatinine > 98th percentile) in < 1/3 of children with MCD, typically mild
Due to reduced glomerular hydraulic conductivity secondary to loss of filtration slit pores, which are responsible for allowing flux of small molecules
Treatment
Drugs
Corticosteroids
90-95% respond over 4-6 weeks
8-week course of steroids often used as 1st treatment of nephrotic syndrome in children
If no response to steroids, renal biopsy typically performed to rule out other diseases
Up to 50% of children and 30% of adults relapse after steroid treatment within 1st year; usually treated with another course of steroids
2nd line of treatment for steroid failures
Alkylating agents (e.g., chlorambucil or cyclophosphamide)
Levamisole
Cyclosporine
Prognosis
Primary (idiopathic)
Rarely, if ever, leads to renal failure
Before steroids and antibiotics, fatalities from infection
Adults with MCD and acute renal failure also usually fully recover
Secondary
Remits if underlying condition can be cured
MCD may be initial manifestation of focal segmental glomerulosclerosis (FSGS) (˜ 5%), in which case prognosis is that of FSGS
MACROSCOPIC FEATURES
MICROSCOPIC PATHOLOGY
Histologic Features
Glomeruli
Normal appearance by light microscopy
Slight increases in mesangial cellularity and matrix in minority
Glomerular basement membranes are normal
Podocytes may be swollen and prominent with basophilic cytoplasm, resembling plasma cells
Resorption droplets in visceral epithelial cells
Loss of normal negative charge revealed by decreased colloidal iron stain of podocytes
Globally sclerotic glomeruli may be seen in MCD in adults
10% of glomeruli may be sclerotic by age 40 and 30% by age 80
In children, involuted glomeruli are sometimes present
Lack of atrophic tubules indicates developmental rather than acquired glomerular sclerosis
Tubules
Protein resorption droplets (“hyaline droplets”)
PAS(+) and red on trichrome stain
Lipid droplets
Origin of term “lipoid nephrosis”
Clear vacuoles on H&E, PAS, and trichrome
Red droplets on oil red O stained frozen sections
Usually little to no tubular atrophy
Older patients with concurrent arteriosclerosis may have underlying glomerular obsolescence and tubular atrophy
Tubular regenerative changes and injury in adults with acute renal failure
Interstitial inflammation and fibrosis are usually absent
Interstitial foam cells may be seen but are rare
ANCILLARY TESTS
Immunofluorescence
Typically no deposits of immunoglobulin or complement
Minority have faint (≤ 1+) staining in glomeruli for IgM ± C3
< 5% of MCD cases have mesangial staining for IgG, IgM, IgA, C1q, &/or C3, particularly in children
Prognosis may be worse in these cases, with higher rate of steroid resistance
Paramesangial pattern suggests nonspecific entrapment
Renal tubular resorption droplets stain for albumin
Usually, there is little immunoglobulin or C3 droplets in tubules (variable)
Electron Microscopy
Transmission
Podocyte foot process effacement (FPE) is widespread and the only major change by EM
Usually, FPE is diffuse and severe, involving > 75% of capillary surface
“Effacement” preferred to “fusion” since foot processes retract rather than fuse and cell body spreads on GBM
Extent of FPE (% of surface) correlates with severity of proteinuria
Filtration slit diaphragms are lost
After remission, foot processes return to normal
Although FPE is primary feature of MCD, it occurs in any renal disease with severe glomerular proteinuria
Podocytes may be “swollen”
Vacuolization and microvillous transformation
Contain resorption droplets and increased cellular organelles
Mild mesangial expansion in minority of cases
Vague mesangial and paramesangial electron densities may be seen, representing nonspecific protein insudation rather than true immune complex deposition
Tubules
Proximal tubules contain electron-dense resorption droplets (secondary lysosomes) and electron-lucent lipid droplets
Immunohistochemistry
Decreased nephrin along GBM, corresponding with loss of slit diaphragms
Nephrin loss is seen in other diseases with FPE, and this stain is not routinely performed
DIFFERENTIAL DIAGNOSIS
Focal Segmental Glomerulosclerosis (FSGS)
Serial sectioning required to detect sclerotic glomeruli to diagnose or exclude FSGS
Segmental hyalinosis or synechiae to Bowman capsule indicative of FSGS
Endocapillary foam cells are rare in MCD and should raise possibility of FSGS
Sclerotic glomeruli in FSGS are most common at corticomedullary junction
Sections of segmentally sclerotic glomeruli may appear normal if plane of section does not include segmental sclerosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree