Microscopic Polyangiitis
Surya V. Seshan, MD
Key Facts
Terminology
Necrotizing vasculitis, with few or no immune deposits, affecting small arteries (capillaries, venules, or arterioles)
Necrotizing glomerulonephritis is common
Etiology/Pathogenesis
ANCA-mediated small vessel vasculitis
Cell-mediated immune mechanism
Clinical Issues
Rapidly progressive or oliguric acute renal failure
Pulmonary hemorrhage
p-ANCA/anti-myeloperoxidase positive (60%)
c-ANCA/anti-PR3 positive (15%)
Renal (90-100%), lung (25-55%)
Microscopic Pathology
Crescentic glomerulonephritis with fibrinoid necrosis
Vasculitis
Not always present, even in multiple levels
Rarely, isolated tubulointerstitial inflammation
No significant granulomatous inflammation
IF: Fibrin in crescents but little or no IgG, IgA, or IgM
Linear IgG in GBM indicates concurrent anti-GBM disease
EM: Rare deposits, breaks in GBM
Top Differential Diagnoses
Granulomatosis with polyangiitis (Wegener) and Churg-Strauss syndrome
Immune complex-mediated glomerulonephritis
Anti-GBM disease
TERMINOLOGY
Abbreviations
Microscopic polyangiitis (MPA)
Synonyms
Microscopic polyarteritis
p-ANCA mediated small vessel vasculitis
Systemic or renal limited crescentic glomerulonephritis
“Pauci-immune” glomerulonephritis
Definitions
Chapel Hill Consensus Conference
Necrotizing vasculitis, with few or no immune deposits, affecting small vessels (i.e., capillaries, venules, or arterioles)
Necrotizing arteritis involving small and medium-sized arteries may be present
Necrotizing glomerulonephritis is very common
Pulmonary capillaritis often occurs
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Higher rate of onset in winter than summer
Similar to granulomatosis with polyangiitis (Wegener)
Pathogenesis
Anti-neutrophil cytoplasmic antibody (ANCA)-mediated small vessel vasculitis
Mainly autoantibodies to antigen myeloperoxidase (p-ANCA)
Minority have autoantibodies to antigen proteinase 3 (c-ANCA)
Subset of MPO-ANCA small vessel vasculitis is renal-limited necrotizing crescentic glomerulonephritis
Subset are ANCA(-) renal-limited necrotizing crescentic glomerulonephritis
Cell-mediated immune mechanism with T-lymphocytes, neutrophils, and histiocytes are necessary for development of crescentic glomerulonephritis
ANCA-activated neutrophils tend to adhere to activated microvascular endothelium to initiate injury
Alternate pathway of complement has been shown to initiate and enhance endothelial injury and vasculitis
CLINICAL ISSUES
Epidemiology
Incidence
Varies with geographic locations
1-8/1,000,000 in Europe and United States
10-24/1,000,000 in Asian and Arab countries
Age
All ages affected
Average age at onset is 50 years
Ethnicity
Geographic variations may be related to ethnic background
Presentation
General
Pulmonary renal syndrome
Constitutional symptoms (up to 75%)
Fever, weakness, weight loss
Arthralgias, myalgias (25-50%)
Hypertension
Renal (90-100%)
Kidney is common organ involved in MPA
Hematuria
Proteinuria
Renal insufficiency
Rapidly progressive or oliguric acute renal failure
Skin
Purpuric rash, palpable (45%)
Lung (25-55%)
Hemoptysis
Dyspnea
Pulmonary hemorrhage
Lung infiltrates
Gastrointestinal (50%)
Abdominal pain
Severe form with bowel perforation
Hepatomegaly
Neurologic (30%)
Peripheral neuropathy less frequent than PAN
Central nervous system
Ear, nose, throat (30-35%)
Mouth ulcers
Epistaxis
Sinusitis
Laboratory Tests
Anemia (normochromic normocytic)
Elevation of acute phase proteins
Erythrocyte sedimentation rate
C-reactive protein
Leukocytosis and thrombocytosis
Rheumatoid factor (39-50%)
Antinuclear antibodies (21-33%)
p-ANCA/anti-myeloperoxidase positive (60%)
c-ANCA/anti-PR3 positive (15%)
Renal
Urinalysis shows red cells and RBC casts
Varying degrees of proteinuria
Elevated serum BUN and creatinine levels
Treatment
Remission induction, remission maintenance, and relapse treatment are 3 phases of therapy
Corticosteroids combined with cyclophosphamide is most common induction protocol
Other forms of immunosuppressive therapy in refractory cases (10%)
Oral cyclophosphamide, mycophenolate mofetil, or azathioprine used for remission maintenance
Prognosis
Severe form of glomerular disease with aggressive course
1-year mortality rate of untreated cases is 80%
Early deaths are usually due to fulminant renal disease and lung hemorrhage in MPA
Frequent relapses occur (25-35%)
Different or new organs may be involved during relapses
Often associated with rash and arthralgias
Generally less severe
Induction protocol
Improvement in > 90% of patients
Complete remission in > 75%
Independent factors that correlate with worse prognosis are older age, higher initial serum creatinine, and pulmonary hemorrhage
Pathologic parameters representative of recovery of renal function include percent of normal glomeruli at initial biopsy, tubular injury, glomerular crescents, and interstitial inflammation
MACROSCOPIC FEATURES
General Features
Normal or mildly increased kidney size
Infarcts when present are small
Petechial hemorrhages
Focal or diffuse
Represent glomerular necrosis; hemorrhage in Bowman space or within tubular lumina
MICROSCOPIC PATHOLOGY
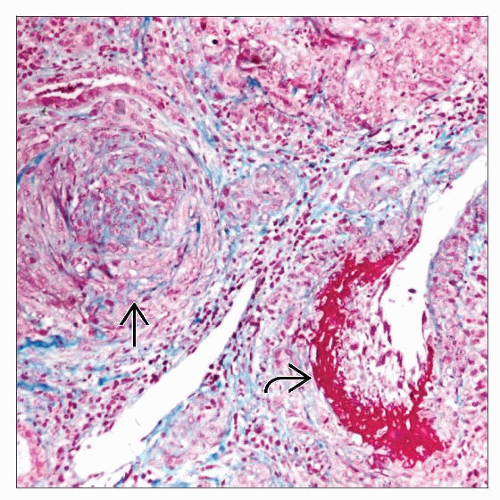
Histologic Features
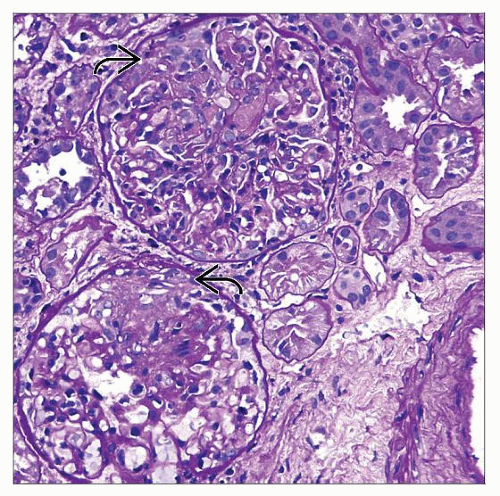
Glomeruli
Pauci-immune crescentic glomerulonephritis
Segmental or, rarely, global glomerular necrosis (80-100%)
Disruption of glomerular basement membranes with accumulation of eosinophilic/fuchsinophilic fibrinoid material
Majority of glomeruli have crescents (average 45-55%), which frequently accompany necrosis
Segmental to extensive lysis of Bowman capsule in severe necrotizing glomerular lesions
Sometimes mild to moderate endocapillary hypercellularity with neutrophils and macrophages
Active periglomerular inflammation of varying intensity composed of lymphocytes, neutrophils, eosinophils, and histiocytes
Periglomerular granulomatous reaction is unlike that seen in granulomatosis with polyangiitis (Wegener)
Subacute or chronic glomerular lesions display fibrocellular or fibrous crescents
Segmental and global glomerular necrosis heals by sclerosis
Sclerosing glomerular changes are accompanied by tubular atrophy and interstitial fibrosis
Tubules and interstitium
Active disease often associated with acute tubulointerstitial inflammation
Rare isolated tubulointerstitial inflammation is noted without glomerular lesions in kidney biopsy
No significant granulomatous inflammation is noted
Renal and extrarenal vessels
Interlobular arteries, smaller arteries, arterioles, capillaries, and venules are affected
Segmental or circumferential fibrinoid necrosis
Palisading mild to intense active inflammatory reaction around necrotic areas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree