MHRA: Licensing, Inspection and Enforcement for Human Medicines
Overview of the Medicines and Healthcare Products Regulatory Agency Group
In 2002, Ministers announced that the Medicines Control Agency and the Medical Devices Agency would be merged to form the Medicines and Healthcare products Regulatory Agency (MHRA). MHRA is responsible for regulating all medicines and medical devices in the UK by ensuring they work and are acceptably safe.
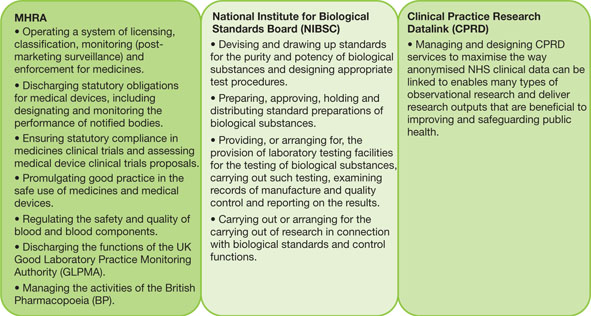
On the 1 April 2013 the National Institute for Biological Standards and Control (NIBSC), previously part of the Health Protection Agency (HPA), became a new centre of the Medicines and Healthcare Products Regulatory Agency Group alongside the Clinical Practice Research Datalink (CPRD).
MHRA and NIBSC have worked closely together for many years and have common interests in managing risks associated with biological medicines, facilitating development of new medicines safely and effectively, and maintaining UK expertise and ability to contribute to assuring the quality and safety of medicines in Europe and beyond.
These developments have created a new organisation that is a world leader in supporting science and research and the regulation of medicines and medical devices, strengthening the support provided to the UK’s medicine’s industry. The new Medicines and Healthcare Products Regulatory Agency group consists of:
● MHRA Regulatory, who protect health and improve lives by ensuring that medicines and medical devices work, and are acceptably safe; focusing on the core activities of product licensing, inspection and enforcement, and pharmacovigilance.
● The Clinical Practice Research Datalink (CPRD), which gives access to an unparalleled resource for conducting observational research and improving the efficiency of interventional research, across all areas of health, medicines and devices. CPRD joined the MHRA in 2012.
● The National Institute for Biological Standards and Control, world leaders in assuring the quality of biological medicines through product testing, developing standards and reference materials and carrying out applied research.
Medicines and Healthcare Products Regulatory Agency
All licensed human medicines available in the UK are subject to rigorous scrutiny by MHRA before they can be used by patients. This ensures that human medicines meet acceptable standards on safety, quality and efficacy. It is the responsibility of MHRA and the expert advisory bodies set up by the Human Medicines Regulations 2012 [SI 2012/1916] (previously under the 1968 Medicines Act) to ensure that the sometimes difficult balance between safety and effectiveness is achieved. MHRA experts assess all applications for new human medicines to ensure they meet the required standards. This is followed up by a system of inspection and testing which continues throughout the lifetime of the medicine.
As the UK government’s public health body which brings together the regulation of human medicines and medical devices, science and research the roles of MHRA are to:
● license medicines, manufacturers and distributors;
● register brokers of finished medicines and manufacturers, importers and distributors of active substances;
● regulate medical devices;
● approve UK clinical trials;
● monitor medicines and medical devices after licensing;
● ensure the safety and quality of blood;
● tackle illegal activity involving medicines, medical devices and blood;
● promote an understanding of the benefits and risks;
● facilitate the development of new medicines;
● support innovation in medicines and medical devices;
● be a leading provider of data and data services for healthcare research;
● work with international partners on issues; and
● provide a national voice for the benefits and risks of medicines, medical devices and medical technologies.
MHRA also hosts and supports a number of expert advisory bodies, including the Commission on Human Medicines (which replaced the Committee on the Safety of Medicines in 2005), and the British Pharmacopoeia Commission. In addition, as part of the European system of medicines approval, MHRA or other national bodies may be the Rapporteur or Co-rapporteur for any given pharmaceutical application, taking on the bulk of the verification work on behalf of all members, while the documents are still sent to other members as and where requested.
One of the key objectives of MHRA is to support greater access to safe and effective medicinal products and medical devices. The timely introduction of innovative products benefits both patients and the public. This section provides information about MHRA’s Innovation Office and highlights how you can get scientific and regulatory advice to support the development of innovational products.
MHRA’s Innovation Office helps organisations that are developing innovative medicines, medical devices or using novel manufacturing processes to navigate the regulatory processes in order to be able to progress their products or technologies. Examples of innovative products include Advanced Therapy Medicinal Products (ATMPs), nanotechnology, stratified medicines, novel drug/device combinations and advanced manufacturing.
If you are a pharmaceutical researcher, developer, manufacturer, etc. and you have a question about an innovative medicine, device or novel manufacturing process, contact the MHRA Innovation Office using one of the routes below.
After contacting the office you will receive a response within 20 working days. Depending on the nature of the query, your response will consist of either a simple answer or a recommended course of action, which may involve regulatory or scientific advice.
Scientific and Regulatory advice
MHRA offers regulatory and scientific advice. For medicines, we currently carry out over 250 scientific advice meetings a year. Joint meetings can be held with the National Institute for Health and Care Excellence (NICE) to consider health technology assessment issues at the same time.
The European Medicines Agency (EMA) offers a comprehensive scientific advice service, available to provide assistance during the initial development of a medicine and during the post-authorisation phase. The advice is provided by the EMA’s Committee for Medicinal Products for Human Use (CHMP),1 based on recommendations of the Scientific Advice Working Party (SAWP).2 Further advice on accessing scientific advice can be obtained from the EMA.3
Scientific advice from the UK
MHRA offers a comprehensive scientific advice service which can assist companies in making decisions about a range of scientific and regulatory issues. Scientific advice can be requested at any stage of the initial development of a medicine and also during the pre-submission period. Please see MHRA webpages on ‘Scientific Advice’.4
MHRA supporting innovation in medicines
MHRA supports innovation through:
Medicines
● membership on European committees (Commission on Human Medicinal Products (CHMP), CAT, COMP, PDCO) and CHMP Working Parties;5
● membership of European Good Distribution Practice (GDP)/Good Manufacturing Practice (GMP) Inspectors Working Group;
● advice given to EMA Innovation Task Force on a wide range of innovative technologies and products;
● working within the ICH network;
● writing regulatory and scientific guidance documents via the ICH and CHMP; and
● membership of European GDP/GMP Inspectors Working Group
Devices sector
● membership of European committees such as the Medical Devices Expert group (MDEG), Borderlines and Classification Group, New and Emerging Technologies Working Group (NET); and
● part of the International Medical Device Regulators Forum.
Inspection, Enforcement and Standards Division
MHRA’s Inspection, Enforcement and Standards Division is responsible for ensuring compliance with the regulations and standards that apply to the manufacture, control and supply of medicines on the UK market.
The Inspectorate Group in MHRA’s Inspection, Enforcement and Standards Division is comprised of dedicated units for Good Manufacturing Practice (GMP), Good Distribution Practice (GDP), Good Laboratory Practice (GLP), Good Clinical Practice (GCP) and Good Pharmacovigilance Practice (GPvP).
Good Manufacturing Practice (GMP)
GMP Inspectors conduct inspections of pharmaceutical manufacturers and other organisations to assess compliance with EC guidance on Good Manufacturing Practice (GMP) and the relevant details contained in marketing authorisations and Clinical Trials Authorisations. They ensure that medicines supplied in the UK and wider EU meet consistent high standards of quality, safety and efficacy. Overseas manufacturing sites to be named on UK or EU marketing authorisations are also required to pass an inspection prior to approval of the marketing authorisation application. Following approval, a risk-based inspection programme maintains on-going surveillance of UK and overseas manufacturing site compliance with EC GMP.
GMP Inspectors are responsible for inspecting and authorising a range of manufacturers of sterile and non-sterile dosage forms, biological products, investigational medicinal products, herbal products and active pharmaceutical ingredients, in addition to certain analytical laboratories. The manufacture of unlicensed medicines by holders of Manufacturer “Specials” Licences in the UK NHS and commercial sector is also inspected on a routine basis to assess compliance with relevant legislation and GMP.
The safety and quality of human blood for transfusion, or for further manufacture into blood-derived medicines, is ensured through inspections of relevant collection, processing, testing and storage activities at Blood Establishments and UK Hospital Blood Banks. These inspections assess compliance with specific UK and EU regulatory requirements, which take into account the detailed principles of GMP.
GMP Inspectors serve on a number of UK, EU and international technical and standards committees and provide help and advice to senior managers, Ministers and colleagues across the Agency, as necessary. Support and expertise is also provided to the inspection programmes of the European Medicines Agency (EMA), European Directorate for Quality of Medicines (EDQM), and the World Health Organization (WHO).
Good Distribution Practice (GDP)
GDP Inspectors conduct inspections of sites of wholesale dealers to assess compliance with EU Guidelines on Good Distribution Practice (GDP) and the conditions of a wholesale dealer’s licence.
Inspectors will ensure that medicinal products are handled, stored and transported under conditions as prescribed by the marketing authorisation or product specification.
Inspections are undertaken of new applicants and then subsequently on a routine schedule based on a risk assessment of the site.
There are a number of developments that had an impact on GDP during 2013 and going forward including:
● the Human Medicines Regulations 2012 [SI 2012/1916] which came into force in August 2012, replacing the majority of the Medicines Act 1968 and its supporting legislation;
● the transposition of the Falsified Medicines Directive 2011/62/EU into UK medicines legislation which extends GDP to any person or entity who procures, stores or supplies medicinal products, for export to countries outside of the EEA and to brokers of finished medicines within the EEA.
● the application of the revised EU Guidelines on GDP of the 5 November, which entered into force on 24 November 2013. This version replaced the earlier version, which entered into force on 8 September 2013, and introduced the following changes:
– the maintenance of a quality system setting out responsibilities, processes and risk management principles in relation to wholesale activities;
– suitable documentation which prevents errors from spoken communication;
– sufficient competent personnel to carry out all the tasks for which the wholesale distributor is responsible;
– adequate premises, installations and equipment so as to ensure proper storage and distribution of medicinal products;
– appropriate management of complaints, returns, suspected falsified medicinal products and recalls;
– outsourced activities correctly defined to avoid misunderstandings;
–
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


