Metastatic Tumors to the Skin
Christine J. Ko, MD
David Cassarino, MD, PhD
Key Facts
Clinical Issues
Cutaneous metastases often located near primary tumor site
Incidence rate of ˜ 2-10% in patients with internal malignancy
Breast cancer metastasizes to skin most frequently
In most cases, skin metastases present after primary tumor has been diagnosed
Very poor prognosis
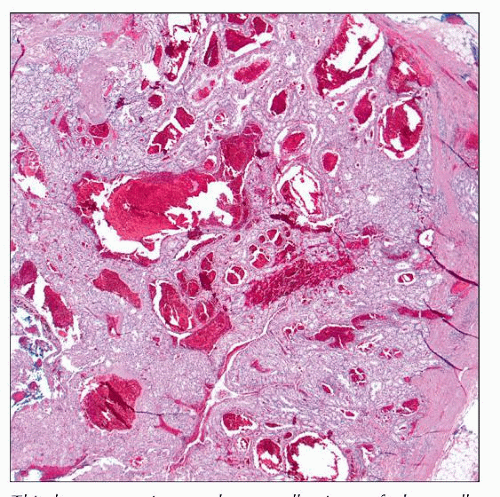
Microscopic Pathology
Many metastases represent adenocarcinoma
Irregular collections of cells, often with lumina
Ancillary Tests
“Organ-specific” markers include PSA, TTF-1, CDX-2, and RCC
Cytokeratin 7 (CK7) and cytokeratin 20 (CK20)
Traditionally, these stains helpful in narrowing down origin of metastatic carcinoma
Cytokeratin 5/6, p63, podoplanin/D2-40
Positivity with these stains supports a primary cutaneous origin over a metastasis
Top Differential Diagnoses
Metastatic adenocarcinoma
Primary adnexal tumors of skin: Generally positive with p63, cytokeratin 5/6, podoplanin
Metastatic renal cell carcinoma
Clear cell hidradenoma and hidradenocarcinoma
Metastatic small cell carcinoma of the lung
Main differential is with primary cutaneous Merkel cell carcinoma
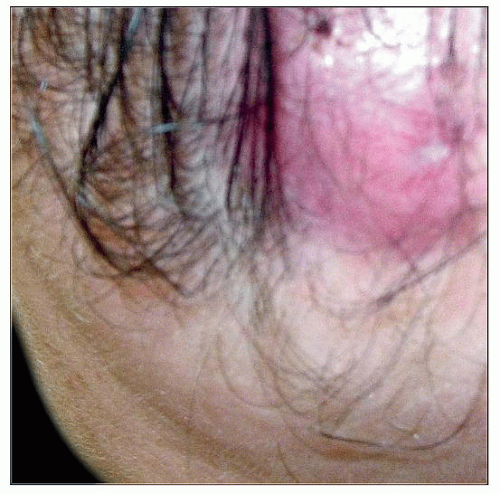 This patient presented with a pink nodule on the anterior scalp. Certain tumors, like renal cell carcinoma (RCC), have the tendency to metastasize to the scalp. |
ETIOLOGY/PATHOGENESIS
Mode of Metastasis
Hematogenous spread
Lymphatic spread
Direct extension from primary tumor
Accidental implantation during surgical procedure
Described with oral cavity, laryngeal, lung, mesothelioma, renal cell, colorectal cancers and others
CLINICAL ISSUES
Epidemiology
Gender
Male: Primary tumor most often lung, colon
Female: Primary tumor most often breast, colon
Site
Cutaneous metastases often located near primary tumor site
Breast carcinoma: Chest wall
Lung carcinoma: Chest wall
Genitourinary carcinoma: Abdominal wall, rarely genitalia
Oral cavity: Head and neck
Scalp
Tumors with a predilection to metastasize to scalp
Thyroid
Breast
Kidney
Lung
Umbilicus: Sister Mary Joseph nodule
Associated with adenocarcinoma of stomach, pancreas, ovary, and others
Presentation
General points
Incidence rate of ˜ 2-10% in patients with internal malignancy
Rare among skin tumors (˜ 2% of all skin tumors)
Patients generally of age 60 or above, but exceptions occur
In neonates, neuroblastoma or other small round blue cell tumors may metastasize to skin
Skin metastases usually present within 2-3 years of diagnosis of primary
Breast cancer metastasizes to skin most frequently
Other internal cancers with not infrequent skin metastases include lung, colorectal, ovarian, head and neck, renal cell carcinoma, and gastrointestinal cancer
Signs/symptoms
Appearance
Generally red-pink, 1-3 cm firm nodule
Deeper purple or “vascular” appearance has been described for renal cell carcinoma metastasis
Multiple or solitary
Clustered or randomly distributed
May be movable or fixed, sometimes ulcerated
Uncommon bullous or inflammatory patterns of metastasis
Asymptomatic or painful
Special clinical variants
Inflammatory (erysipeloid) carcinoma
Lymphatic spread of carcinoma
Warm, red, tender plaque; resembles erysipelas
Most commonly associated with breast carcinoma, but also may be due to other carcinomas (i.e., colon, prostate) and melanoma
Carcinoma telangiectoides
Secondary to breast carcinoma
Plaque of coalescing telangiectasias and erythematous papules
Carcinoma en cuirasse
Secondary to breast carcinoma
Skin hardened and leathery
Superior vena cava syndrome
Can be secondary to lung carcinoma
Obstruction of superior vena cava leads to edema, cyanosis, plethora of head/neck; subcutaneous vessels may be prominent
Sister Mary Joseph nodule
Classically described as red nodule on umbilicus, most commonly due to gastric carcinoma
Alopecia neoplastica
Localized patches of alopecia on scalp secondary to metastatic disease in dermis
Laboratory Tests
Ovarian cancer
High CA-125 suggestive of advanced disease
CA 19-9 may be elevated
Colon cancer
CEA may be used to monitor disease
Hepatocellular and testicular cancer (and some others)
α-fetoprotein may be elevated
Pancreatic cancer
CA 19-9 may be elevated
Gastric cancer
CA 19-9 may be elevated
Prostate cancer
Prostate-specific antigen (PSA) often elevated
Natural History
Skin metastases are rarely presenting clue to internal malignancy
In most cases, skin metastases present after primary tumor has been diagnosed
Treatment
In advanced disease, excision of metastases may be palliative
Other treatment options dependent on type of tumor and extent of disease (e.g., chemotherapy or radiation)
Chemotherapy
Traditional drugs (e.g., anthracyclines, taxanes)
Trend is to test tissue for molecular targets, and if positive, use targeted treatment (e.g., trastuzumab in Her2-neu positive breast cancer, tamoxifen in estrogen receptor positive cancers)
Prognosis
Poor overall survival
One study cites range of 1-34 months
MICROSCOPIC PATHOLOGY
Histologic Features
Many metastases represent adenocarcinoma: Irregular collections of cells in dermis, often forming lumina
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree