Metabolic Surgery and Intestinal Bypass for Hypercholesterolemia
Henry Buchwald
Metabolic Surgery and the Metabolic Syndrome
In 1978, Richard L. Varco and I published a book titled Metabolic Surgery, in which we defined metabolic surgery “as the operative manipulation of a normal organ or organ system to achieve a biological result for a potential health gain.” This discipline has actually been practiced for nearly 100 years. The most popular seminal application was peptic ulcer surgery, where various gastrectomies and vagal nerve interventions, carried out on normal tissues, were devised to cure pyloric and duodenal ulcer pathology, which itself remained surgically untouched. Intestinal metabolic surgery originated in 1953 to 1954 with the advent of the jejunoileal bypass for morbid obesity. Over the years, this was followed by gastric bypass, constriction, resection, and distention procedures, as well as gastric and vagal electrical stimulation, independent or in concert with intestinal bypasses, transpositions, resections, and intraluminal barriers—all to achieve weight loss and to ameliorate the comorbidities of obesity.
About 15 years ago, the term Metabolic Syndrome was added to the lexicon of diseases. This complex of independent entities was defined as consisting of obesity, type 2 diabetes mellitus, hypertension, and hyperlipidemia. Once designated a syndrome by internists, the nonsurgical specialties have searched for a treatment(s) and a cure, often failing to recognize that bariatric surgery, or more precisely metabolic/bariatric surgery, can resolve essentially all of the manifestations of the metabolic syndrome. It should be stated that the so-called metabolic syndrome has not been identified with a specific etiologic agent, and, in the light of current knowledge, can be thought to include the primary disease of obesity and three of its comorbid conditions.
In this chapter, we will concentrate on a metabolic surgery procedure—the partial ileal bypass—that was developed specifically for the management of hyperlipidemia, one aspect of the metabolic syndrome, and that does not engender noticeable weight loss.
Basic Research Antecedents
The first partial ileal bypass operation specifically for reduction of circulating cholesterol was performed on May 29, 1963. Since then, the series has grown to approximately 600 patients, and the operation has been performed by many others throughout the world. This procedure was used in a multi-institutional secondary atherosclerosis intervention trial funded by the National Heart, Lung, and Blood Institute in 1972, designated the Program on the Surgical Control of the Hyperlipidemias (POSCH). This study has been the only surgical randomized clinical trial to test the efficacy of cholesterol lowering in the management of atherosclerosis and its clinical manifestations, and the first of the statistically significant trials confirming the clinical benefits of cholesterol, in particular low-density lipoprotein (LDL) cholesterol reduction.
The rationale for partial ileal bypass is interference with the enterohepatic cholesterol and bile acid cycles to achieve a direct loss of cholesterol from the body and an indirect cholesterol drain by the forced conversion of part of the cholesterol pool to bile acids. This hypothesis has been confirmed in the laboratory and by clinical investigation.
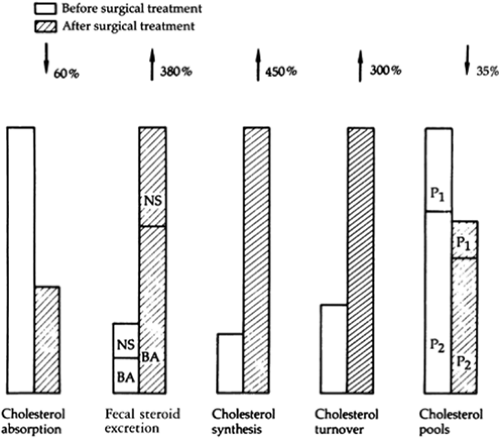
In 1963 my associates and I devised a method of measuring cholesterol absorptive capacity using blood radioactivity levels after a standard oral test dose of 14C-4-cholesterol in butter. In 30 patients studied before and 3 months after partial ileal bypass, the cholesterol absorptive capacity was reduced an average of 60% (Fig. 1). Cholesterol absorptive capacity was retested in certain of these patients at intervals throughout the follow-up period. No trend to return to the preoperative cholesterol absorptive capacity was noted. Fecal steroid excretion was measured in selected patients before and after partial ileal bypass, using an isotope balance technique after a single intravenous injection of 14C-4-cholesterol. After
the operation, a 3.8-fold increase was seen in total fecal sterol excretion, with a much greater increase in bile acids than in neutral steroids (Fig. 1). The same magnitude of sterol excretion was observed in patients studied 1 year after the operation, demonstrating the apparently lasting effect of ileal bypass on fecal sterol excretion.
the operation, a 3.8-fold increase was seen in total fecal sterol excretion, with a much greater increase in bile acids than in neutral steroids (Fig. 1). The same magnitude of sterol excretion was observed in patients studied 1 year after the operation, demonstrating the apparently lasting effect of ileal bypass on fecal sterol excretion.
Using an in vivo method for estimating cholesterol biosynthesis based on the incorporation of tritium from body water into plasma cholesterol, we showed a 5.7-fold increase in cholesterol synthesis at 3 months and at 1 year (Fig. 1). Direct and indirect methodologic confirmation of these results has been offered by Miettinen and Moutafis. Understandably, the isotopic cholesterol turnover rate increases approximately threefold after this procedure (Fig. 1). Finally, using a method similar to that of Goodman and Noble, we calculated the freely miscible, slowly miscible, and total exchangeable cholesterol pools before and 1 year after partial ileal bypass. The total miscible pool was reduced by nearly one-third, and in each patient a relatively greater reduction was seen in the slowly miscible cholesterol pool than in the freely miscible pool, which suggests a loss of cholesterol from tissues other than the blood, liver, and intestinal mucosa (Fig. 1).
There is also information available from the laboratory with respect to partial ileal bypass and the management of atherosclerosis. In adult and infant cholesterol-fed rabbits, my associates and I demonstrated not only prevention of atherosclerosis by partial ileal bypass but also reduction of the lipid content of established atherosclerotic plaques concurrent with their evolution from the proliferative phase to a healing phase.
Atherosclerosis and Hypercholesterolemia
Atherosclerosis is an ancient disease. Autopsies of Egyptian mummies have disclosed severe arterial occlusive disease. From clinical obscurity through the centuries, atherosclerosis has come to the forefront during the past 50 years. Atherosclerosis today remains the most common serious affliction in the Western world, and its complications, such as myocardial infarction and peripheral vascular disease, are the leading causes of death in industrialized countries. Approximately 600,000 deaths from coronary heart disease occur in the United States yearly. The deaths from cardiac, cerebral, and peripheral atherosclerotic cardiovascular disease in the United States account for approximately half of the national death rate, exceeding the combined rate for cancer, accidents, and all other causes. This disease is not a geriatric problem. Battlefield autopsies from Korea and Vietnam showed that 45% to 77% of young American soldiers killed in action had evidence of coronary atherosclerotic involvement.
In 1847, Vogel showed that cholesterol was a constituent of the atherosclerotic plaque lesion. Subsequently, a long succession of pathologists, clinicians, and epidemiologists have provided undeniable evidence, terminating in the prospective analyses of the last 30 years, for the tenet that circulating cholesterol concentration is a primary, if not the primary, indicator of atherosclerotic risk and more than likely a major causal agent in the formation of the atherosclerotic plaque.
The average lowering of cholesterol concentration obtained by strict dietary management is 3% to 10%. Drug therapy was equally unimpressive until the 1990s and the introduction of the 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors. These statin agents are effective, convenient, and quite safe. Reported side effects of the HMG-CoA reductase inhibitors include changes in bowel function, headaches, nausea, fatigue, insomnia, and skin rashes. Two to three percent of patients have changes in liver function tests that require discontinuation of these agents. Muscle cramps are not rare with these agents, and myositis has been reported. Rhabdomyolysis leading to acute renal failure has occurred in patients treated with HMG-CoA reductase inhibitors in combination with immunosuppressive therapy after cardiac transplantation and in patients treated with a combination of a statin and gemfibrozil.
Open
The open technique for partial ileal bypass has remained essentially unchanged since 1963. Intestinal preparation is carried out the evening before operation, with a clear-liquid diet, nonabsorbable oral antibiotics, and cathartics; enemas are not used. The skin is antiseptically washed preoperatively and in the operating room. An intravenous infusion is started through a central catheter and low molecular weight heparin is given. Intravenous administration of antibiotics is begun at the time of incision (2 g of a cephalosporin) and may be maintained for 24 hours after the operation.
General anesthesia is preferred to a regional block because general anesthesia provides better cardiovascular control, an advantage in these patients, who often have threatening arterial disease. Anesthesiologists prefer a gradual barbiturate induction, intubation, and light inhalation anesthesia with muscle paralysis.
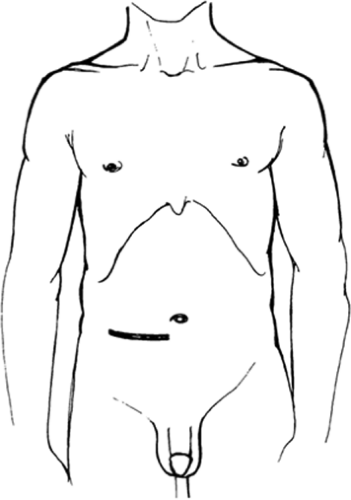
Unless a concomitant procedure is planned, entrance is gained into the abdominal cavity by a right lower quadrant transverse incision approximately 2 cm below the umbilicus (Fig. 2). As a rule, only the right rectus muscle, the linea alba, and a few centimeters of the oblique muscles are divided. General hemostasis and muscle division are performed with the cautery; the inferior epigastric vessels are ligated. The abdomen is carefully explored, and the nasogastric tube placed by the anesthesiologist in the operating room is appropriately positioned along the greater curvature of the stomach by the surgeon, who stands on the right side of the operating table. Antibiotic-soaked laparotomy pads are inserted along the edges of the incision, and a plastic wound protector (5-in diameter) is placed.
The cecum is delivered into the operative field. On occasion, this necessitates cutting the peritoneal reflection at the white line of Toldt posterior and inferior to the cecum and the terminal ileum, and gentle retroperitoneal freeing of these structures. The appendix, if still present, is removed, with ligature of the appendiceal mesenteric vessels, ligature of the stump with 3-0 chromic catgut, inversion of the stump with a 4-0 nonabsorbable purse-string suture, and reinversion of the area with a 4-0 Z stitch.
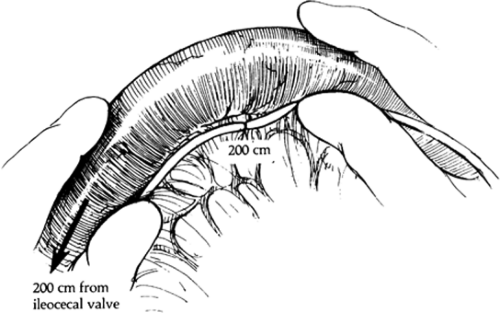
The small intestine is next delivered into the field and measured with a marked umbilical tape knotted every 25 cm. The tape is placed along the mesenteric border of the intestine because this surface is less variable in its dimensions than the antimesenteric length. When the operator, measuring retrograde from the ileocecal valve, reaches 200 cm (Fig. 3), he or she places marking sutures of different colors through avascular windows in the mesentery and around the intestine. Measurement is then continued to the ligament of Treitz, and 25 cm is added for the duodenum to obtain the total length of small intestine. In my experience, the intestinal length has varied from 400 to 700 cm. If the measurement is greater than 600 cm, the marking sutures are moved 50 cm cephalad and the segment to be bypassed is increased from 200 to 250 cm.
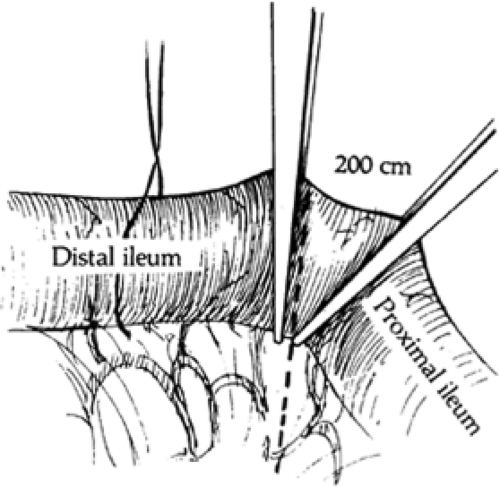
Between the different-colored marking sutures, a small area of mesentery is cleared, with 5-0 Tevdek (braided polyester, Teleflex Medical, Mansfield, MA) ligature of mesenteric vessels if necessary. A Dennis clamp is placed straight across the prepared intestine on the distal side, and a Kocher–Allen clamp is placed at a slight angle on the proximal aspect (Fig. 4). The small intervening segment of intestine is resected, and the ends of the intestine are cauterized at the clamp margins.
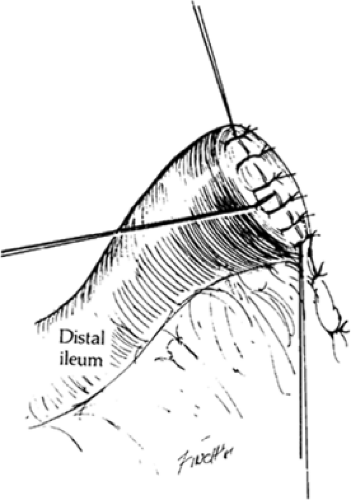
The distal end of this division, or what is to become the proximal end of the bypassed segment, is closed in two layers. I prefer an inner row of 4-0 absorbable Vicryl (polyglactin 910, Ethicon, Inc, Somerville, NJ) sutures, taken in a Parker–Kerr manner, and an outer reinverting row of interrupted 5-0 Tevdek sutures. The two corner and the middle sutures are not cut but are retained for future tacking of the closed end of intestine (Fig. 5).
Anastomosis is then accomplished between the proximal small intestine and the cecum. The cecum is retained to maximize the water-absorbing surface, and anastomosis is made distal to the ileocecal valve to minimize ileal retention of cholesterol and bile acids and their resorption. Anastomosis is made in an end-to-side manner on the anterior taenia approximately 6 cm above the inverted appendiceal stump (Fig. 6). I use a two-layer open anastomosis. The posterior row of interrupted 5-0 Tevdek sutures is placed and, except for the corners, tied and cut. The crushed portion of the ileum is cut off sharply with the clamp, and hemostasis of the fresh surface is obtained by careful use of the cautery. An equidistant incision is made into the cecum, approximately in the middle of the taenia.
A whip-lock inner row of 4-0 Vicryl (Ethicon, Inc, Somerville, NJ) sutures is started in the inferior corner, run to the upper corner, taken around the upper corner, and run back in the Connell manner. The anastomosis is then completed by an anterior row of interrupted 5-0 Tevdek sutures in the Lembert manner, with reinforcement of both corners (Fig. 7).
A whip-lock inner row of 4-0 Vicryl (Ethicon, Inc, Somerville, NJ) sutures is started in the inferior corner, run to the upper corner, taken around the upper corner, and run back in the Connell manner. The anastomosis is then completed by an anterior row of interrupted 5-0 Tevdek sutures in the Lembert manner, with reinforcement of both corners (Fig. 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree