KEY TERMS
Attention deficit hyperactivity disorder (ADHD)
Bipolar disorder (manic-depressive illness)
National Comorbidity Survey (NCS)
Post-traumatic stress disorder (PTSD)
According to the World Health Organization, mental illnesses account for more disability in developed countries than any other group of illnesses, including cancer and heart disease. In 2004, an estimated 25 percent of adults in the United States reported having a mental illness in the previous year.1 Nearly half of adult Americans will develop at least one mental illness during their lifetime.
The most common mental illnesses in adults are anxiety and mood disorders. These disorders are often associated with chronic diseases, including cardiovascular disease, diabetes, asthma, epilepsy, and cancer. People with mental illness have an increased risk of injuries, both intentional and unintentional. They are also more likely than people without mental illness to use tobacco products and to abuse alcohol and other drugs.
Major Categories of Mental Disorders
The categories of mental disorders listed in the 1999 Surgeon General’s report Mental Health are anxiety, psychosis, disturbances of mood, and disturbances of cognition.2 These categories are broad, heterogeneous, and somewhat overlapping. Any particular patient may manifest symptoms from more than one of these categories. Thus mental illnesses are sometimes hard to diagnose and, consequently, hard for epidemiologists to count.
Anxiety
Anxiety is a vitally important physiological response to dangerous situations that prepares one to evade or confront a threat in the environment. However, inappropriate expressions of anxiety exist if the anxiety experienced is disproportionate to the circumstance or interferes with normal functioning. Examples include phobias, panic attacks, and generalized anxiety. Other manifestations of anxiety include obsessive-compulsive disorder and post-traumatic stress disorder (PTSD).
Psychosis
Disorders of perception and thought process are considered to be symptoms of psychosis. They are most characteristically associated with schizophrenia, but psychotic symptoms can also occur in severe mood disorders. Among the most commonly observed psychotic symptoms are hallucinations—sensory impressions that have no basis in reality—and delusions—false beliefs held despite evidence to the contrary, such as paranoia.
Disturbances of Mood
Disturbances of mood characteristically manifest themselves as a sustained feeling of sadness or hopelessness—major depression—or extreme fluctuations of mood—bipolar disorder. Mood disturbances are also associated with symptoms like disturbances in appetite, sleep patterns, energy level, concentration, and memory. Perhaps most alarming, major depression is often associated with thoughts of suicide.
Disturbances of Cognition
The ability to organize, process, and recall information, as well as to execute complex sequences of tasks, may be disturbed in a variety of disorders. Notably, Alzheimer’s disease is a progressive deterioration of cognitive function, or dementia.
Epidemiology
A number of surveys of the U.S. population have yielded estimates of the prevalence of mental illness. The most comprehensive, the National Comorbidity Survey (NCS), conducted from the fall of 1990 to spring of 1992, was sponsored by the National Institute of Mental Health, the National Institute of Drug Abuse, and the W. T. Grant Foundation. Researchers at Harvard Medical School interviewed 10,000 adults asking questions designed to diagnose specific mental and substance use disorders.3 The same respondents were reinterviewed in 2001–2002 to study patterns and predictors of the course of mental disorders and their relation to substance use. The NCS is the source of the commonly cited findings about the high incidence and prevalence of mental illness in the United States.
Some of the surveys conducted by the Centers for Disease Control and Prevention (CDC) include questions on mental health. The Behavioral Risk Factor Surveillance System (BRFSS), a state-based telephone survey, conducts approximately 450,000 adult interviews each year. One question asked every year of all respondents is the number of mentally unhealthy days they experienced. Individual states may choose optional modules, including some that address other mental health issues in depth. For example, in 2006, 2008, and 2010, an optional module included one question on lifetime diagnosis or anxiety and one on lifetime diagnosis of depression.1
The National Health Interview Survey, which conducts in-person interviews with carefully selected representative households, has since 1997 asked a question designed to identify serious psychological distress in the past 30 days. In 2007, the survey included three questions on lifetime diagnoses: “Have you EVER been told by a doctor or other health professional that you had bipolar disorder? Schizophrenia? Mania or psychoses?”1
For the National Health and Nutrition Examination Survey, participants chosen from a carefully selected representative households are asked questions on number of mentally unhealthy days, as well as questions designed to measure depression. A survey of women who have recently given birth, the Pregnancy Risk Assessment Monitoring System (PRAMS) asks questions about postpartum depression. Surveys on healthcare utilization gain information about mental health issues from data provided by hospitals, community health centers, office-based providers, and nursing homes.
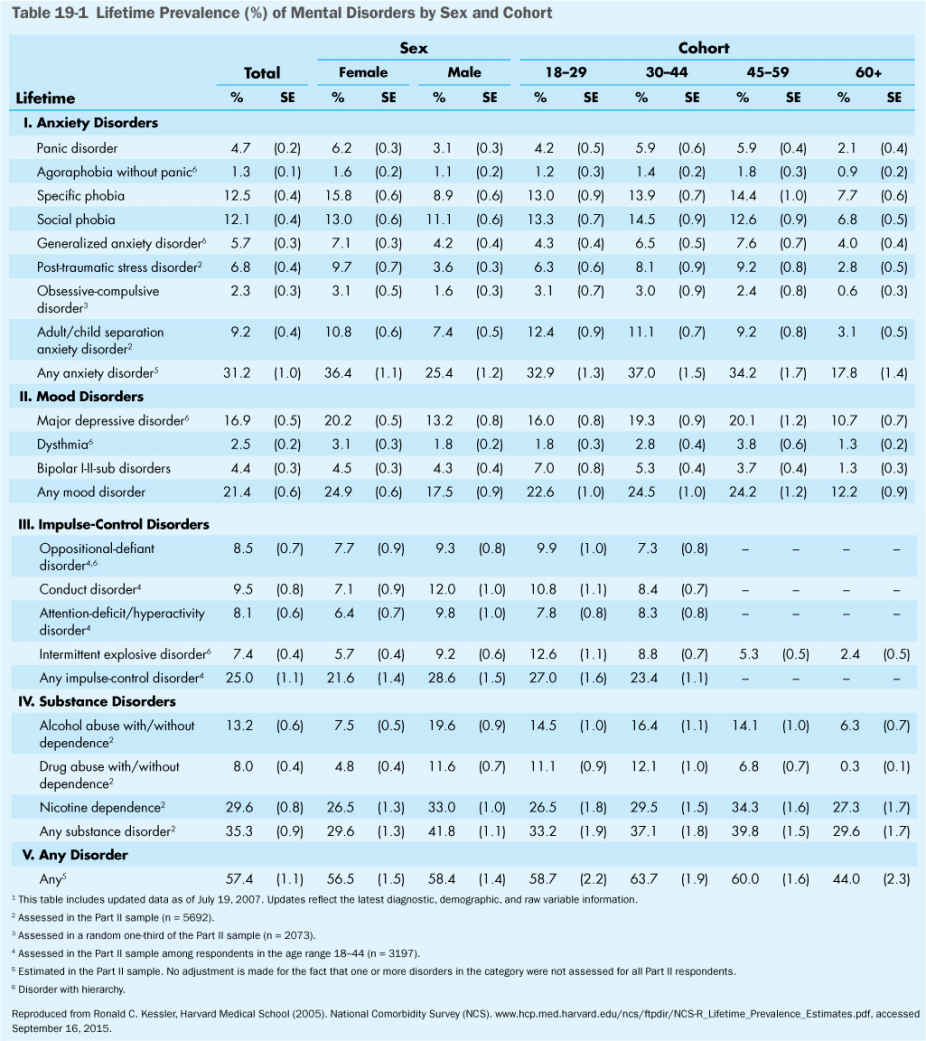
The NCS provides data on the lifetime prevalence of mental disorders broken down by types of disorder—anxiety disorders, mood disorders, impulse-control disorders, and substance disorders—and for each, sex and age cohort of people suffering from each type. The total percentage of the population that has had an anxiety disorder is 31.2 percent; 21.4 percent have had a mood disorder; 25.0 percent an impulse-control disorder; and 35.3 percent a substance disorder. There is significant overlap among the specific disorders, with the total prevalence of any mental disorder amounting to 57.4 percent. (Table 19-1) shows details of the lifetime prevalence of various mental disorders by sex and age group.
When broken down by sex, females reported more anxiety disorders and mood disorders than males, while males have more impulse-control disorders and substance disorders. It is notable that for all the disorders, younger cohorts have a higher prevalence than those over 60 years. In fact, the prevalence of anxiety disorders and mood disorders is only about half among those over 60 as it is among those 18 to 59. Only nicotine dependence is comparable among the older cohort to the younger groups.1
Two CDC surveys (BRFSS and PRAMS) collect data at the state or substate level, and the prevalence of some disorders varies substantially across regions of the country. Southeastern states generally have the highest prevalence of depression, serious psychological distress, and mean number of mentally unhealthy days. This finding likely reflects the association between mental illness and certain chronic diseases, such as obesity, diabetes, and cardiovascular disease, which are also more prevalent in the Southeast.
Causes and Prevention
The precise causes of most mental disorders are not known, but much is known about the broad forces that shape them. The causes of mental disorders are viewed as a product of the interaction between biological, psychological, and sociocultural factors. Genetic factors are important in some mental disorders, including schizophrenia, bipolar disorder, autism, and attention deficit hyperactivity disorder (ADHD). However, in the case of schizophrenia, for example, studies of identical twins find that in only half the cases where one twin has the disorder, does the second twin also have it, even though both twins have the same genes. This implies that environmental factors exert a significant role, and therefore there is a possibility of intervening to prevent the development of the disorder. PTSD is clearly caused by exposure to an extremely stressful event, although not everyone develops PTSD after such exposure. Again appropriate treatment may prevent the disorder.2
Prevention of mental illness may depend on identification of risk factors that can be targeted, especially in children. Risk factors that are common to many disorders include individual factors, family factors, and community factors. An individual may be put at risk by neurophysiological deficits, difficult temperament, chronic physical illness, or below-average intelligence. Family factors that increase risk are severe marital discord, social disadvantage, overcrowding or large family size, paternal criminality, maternal mental disorder, and admission into foster care. Community factors such as living in an area with a high rate of disorganization and inadequate schools may also increase risk.2
Children
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


