46 Menopause
Menopause
Physiological changes
Ovarian
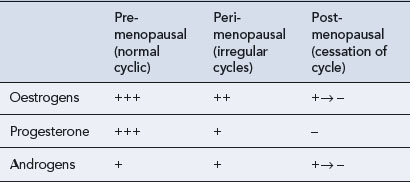
Ovarian function includes two major roles: the production of eggs (gametogenesis) and the synthesis and secretion of hormones (hormonogenesis). Both of these functions undergo subtle changes with ageing so that fewer ova are produced and they are less readily fertilised, and the hormone levels become irregular. It is the granulosa cells in the developing follicle that normally secrete estradiol, and lack of this follicular activity results in diminishing oestrogen secretion. The diminution in the number of active follicles is followed by an increase in follicle-stimulating hormone (FSH) secretion from the anterior pituitary gland as the normal feedback mechanisms between ovarian estradiol secretion and the hypothalamus–pituitary axis become disrupted. It may be that there is an age-related decrease in sensitivity to feedback inhibition that exacerbates this increase in FSH levels. In women who are still bleeding, an FSH level exceeding 10–12 iu/L on day 2 or 3 of the bleed is indicative of a diminished ovarian response. A high FSH level (above 30 iu/L) and a low estradiol level (below 100 pmol/L) in the plasma characterise menopause. The low oestrogen level fails to stimulate growth of the uterine endometrium. As endometrial growth has not occurred, there can be no menstruation (shedding of the endometrium) and this signifies that menopause has arrived. Since ova are not being released, the production of progesterone from the ovary also ceases and the levels of luteinising hormone (LH) eventually rise. Thus, peri-menopausal and menopausal women are subjected to an increasing ovarian hormone deficiency, as shown in Table 46.1.
Bone
Osteoporosis is defined by WHO as a systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue leading to enhanced bone fragility and a consequent increase in fracture risk. In 2006, WHO estimated that it affects 200 million women worldwide. In addition, approximately 30% of women over the age of 50 have one or more vertebral fractures compared with one in five men over the age of 50 who will have an osteoporosis-related fracture in their remaining lifetime. The total number of hip fractures in 1950 was 1.66 million, and by 2050, this figure could reach 6.26 million. Twenty percent of people die within 1 year of a hip fracture (Cooper, 1997). Typical morbidities after a vertebral fracture include:
To contextualise risk, the remaining lifetime probability in women at menopause of a fracture at any one of these sites exceeds that of breast cancer (~12%). Also, the likelihood of a fracture at any of these sites is 40% or more in developed countries (Kanis et al., 2000), a figure close to the probability of coronary heart disease. Risk factors for osteoporosis include low body mass index (<19 kg/m2), smoking, early menopause, family history of maternal hip fracture, long-term systemic corticosteroid use and conditions affecting bone metabolism, especially those causing prolonged immobility. Osteoporosis is most common in white women. People with osteoporosis are at risk of fragility fractures, occurring as a result of mechanical forces which would not ordinarily cause fracture. The clinically relevant outcome in evaluating treatments for osteoporosis is the incidence of fragility fracture as otherwise this condition is asymptomatic and therefore undiagnosed. The most common sites for these fractures are the hip, vertebrae and wrist. In the UK, the combined cost of hospital and social care for patients with a hip fracture amounts to more than £1.73 billion per year (Torgerson et al., 2001). This is very similar to the annual £1.75 billion health care system costs of coronary heart disease costs. The cost of treating all osteoporotic fractures in post-menopausal women has been predicted to increase to more than £2.1 billion by 2020 (Burge, 2001).
Miscellaneous
Thinning of the skin, brittle nails, hair loss and generalised aches and pains are also associated with reduced oestrogen levels (Hall and Phillips, 2005). The skin is the largest non-reproductive target on which oestrogen acts. Oestrogen receptors, predominantly of the ERβ type, are widely distributed within the skin. Both types of oestrogen receptor (ERα and ERβ) are expressed within the hair follicle and associated structures. Thus, epidermal thinning, declining terminal collagen content, diminished skin moisture, decreased laxity and impaired wound healing (selective ERα ligands are being investigated for their wound-healing properties) have been reported in post-menopausal women.
Psychological changes
Older age at menarche and younger age at menopause are associated with poorer cognitive functioning during ageing. Recent studies have demonstrated that sex steroids have a multifarious and complex relationship with the central nervous system (Hogervorst et al., 2009). For example, there may be a positive correlation between increasing parity and improved executive functioning in response to oestrogen. This temporal relationship between oestrogen deprivation and response to exogenous oestrogen was clearly exemplified in the memory study arm of the WHI (Coker et al., 2010) and MWS studies (Hogervorst and Bandelow, 2010) at the turn of the twenty-first century.
Management
Hormone replacement therapy
Oestrogen therapy
There are four main routes of administration for oestrogens in HRT:
The use of oral oestrogen therapy, while convenient for the patient, does mean that the oestrogen will be subjected to conversion to estrone by the liver and the gut, thereby altering the estradiol:estrone ratio in favour of the less active oestrogen, estrone. The oral preparations have different metabolic effects due to first-pass hepatic metabolism. Smoking stimulates metabolism of oestrogens by cytochrome P450 and decreases plasma oestrogen levels by 40–70% in oral oestrogen users. Smoking has no significant effect on plasma oestrogen levels in users of transdermal preparations. Oral delivery compared to transdermal delivery (Table 46.2) also has different effects on lipid levels (Vrablik et al., 2008). In addition, orally administered oestrogens undergo first-pass hepatic metabolism, which may result in some reduction in anti-thrombin III, a potent inhibitor of coagulation. Implants and patches show smaller changes in coagulation, platelet function or fibrinolysis.
Table 46.2 Effect of HRT administration route on lipid profile
| Oral | Transdermal |
|---|---|
| ↓ Low-density lipoprotein | ↓ Low-density lipoprotein |
| ↓ Total cholesterol | ↓ Total cholesterol |
| ↑ High-density lipoprotein | ↔ High-density lipoprotein |
| ↑ Triglycerides | ↓ Triglycerides |
| ↑ Bile cholesterol | ↔ Bile cholesterol |
More constant levels of oestrogen result from the use of transdermal patches containing estradiol, and these have the added advantage of a more physiological estradiol:estrone ratio (Delmas et al., 1999). However, the adhesive used in these transdermal patches and the alcohol base can cause skin irritation. The patch is applied to the non-hairy skin of the lower body, and care should be taken to ensure that it is placed away from breast tissue. The patch is changed either once or twice a week, thus providing a constant reservoir of estradiol to provide a controlled release into the circulation. Estradiol is also available in a gel formulation, applied daily to the skin over the area of a template (to ensure correct dosage), but this formulation may give erratic absorption. The intranasal preparation, administered as a nasal spray, also avoids hepatic first-pass metabolism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree