Membranoproliferative Glomerulonephritis, Type I/III
A. Brad Farris, III, MD
Key Facts
Terminology
Subendothelial electron-dense deposits with mesangial interposition
Clinical Issues
Older children, adolescents, & young adults (˜ 7-30 years old)
Nephrotic syndrome: > 50% of patients
Hematuria: 10-20% with acute nephritic syndrome
Hypocomplementemia
Microscopic Pathology
Lobular, hypercellular glomerulus with thickened capillary walls & increased mesangial substance
“Tram tracks” or duplication of GBM (best seen on PAS & silver stains)
Crescents in ˜ 20% of cases
± neutrophils and monocytes
Hyaline aggregates of immune complexes in capillary lumina
IF: Classic feature is C3 in capillary walls & mesangium, “railroad track,” “lumpy-bumpy” granular C3, IgG, & early complement (C1q & C4)
EM: Large, amorphous dense subendothelial and mesangial deposits in glomerulus
Type III (Burkholder): MPGN, type I + membranous GN (subendothelial + subepithelial deposits)
Type III (Anders and Strife): MPGN, type II (also known as dense deposit disease) + MPGN, type I
Top Differential Diagnoses
Lupus erythematosus
Cryoglobulinemia
Chronic Infections
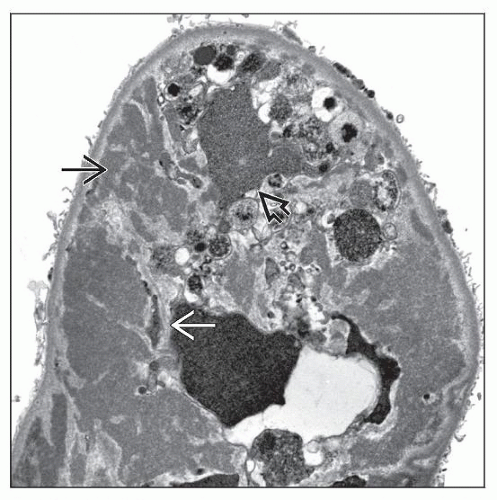
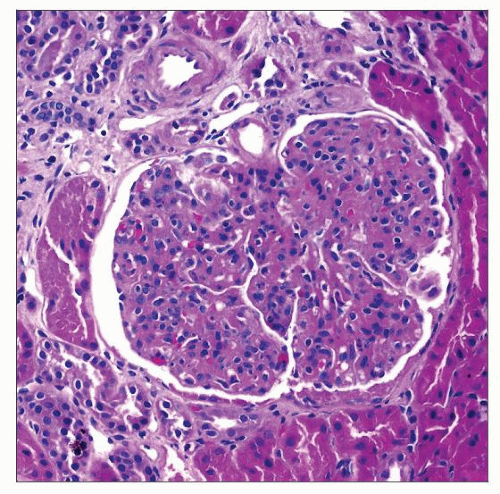 MPGN, type I shows exuberant mesangial hypercellularity, which gives a lobulated appearance and capillary wall thickening, as shown here in a 10-year-old boy with hematuria, proteinuria, and low C3. |
TERMINOLOGY
Abbreviations
Membranoproliferative glomerulonephritis (MPGN)
Synonyms
Hypocomplementemic glomerulonephritis (GN)
Lobular GN
Mesangiocapillary/mesangiopathic GN
Definitions
Subendothelial electron-dense deposits with mesangial interposition between capillary wall and GBM with clinical finding of hypocomplementemia
ETIOLOGY/PATHOGENESIS
Infectious Agents
May occur after infection, particularly upper respiratory tract infection
Autoimmune
± C3 nephritic factor, IgG autoantibody, or other autoantibodies, resulting in persistent activity of alternative complement pathway (˜ 25% of MPGN type I patients)
Immune Complex Deposition
Circulating immune complexes present in many MPGN, type I patients
Activates classical & alternative complement pathways
Chronic serum sickness caused by repeated injection of antigen resembles MPGN
Secondary Causes
Many different etiologies can lead to 2° MPGN-type pattern
Therefore, 1° MPGN is a diagnosis of exclusion
CLINICAL ISSUES
Epidemiology
Incidence
˜ 5% of GN in children and adults
Age
Primarily older children, adolescents, and young adults (˜ 7-30 years old)
Rare in children < 2 years old or adults > 50 years old
Gender
Approximately equal male:female ratio
Ethnicity
Reportedly higher incidence in whites
Navajo Indians in USA may have high rates of nondiabetic ESRD due to GN of this type
Presentation
Nephrotic syndrome
Occurs in > 50% of patients
Predominant feature in 2/3 of patients
Proteinuria
May be subnephrotic
Syndrome often initially nephritic & eventually nephrotic
Hypocomplementemia
Low C3 as in other types of MPGN
Low classic pathway components (C1, C2, and C4), Factor B, and properdin
˜ 80% of MPGN, type I; ˜ 100% of MPGN, type II; & ˜ 50% of MPGN, type III
Hematuria
± recurrent episodes of gross or microscopic hematuria
Acute nephritic syndrome in 10-20%
Hypertension
Usually mild but may be malignant
˜ 1/3 of patients
Renal vein thrombosis may be present
Laboratory Tests
Complement often decreased, as above
In type I MPGN
↓ C3 & total hemolytic complement (CH50) in 50%
C1q, C4, properdin, & factor B borderline/↓ in < 50%
In type III MPGN
↓ C3, normal C4
↓ C5, C6, C7, and C9 levels may be 2° to terminal pathway nephritic factor
C3 nephritic factor (common in type II MPGN)
Present in ˜ 25% of type I MPGN patients & absent in type III MPGN
Treatment
Drugs
Steroids
Long-term, low-dose steroids used in children with 1° MPGN (lead to growth retardation & hypertension)
Repeat biopsy often performed within 5 years of therapy initiation to ascertain if continued therapy is needed
Antiplatelet agents (dipyridamole & aspirin) used alone or with steroids
Prognosis
Variable but usually poor with persistent proteinuria
Classically a chronic, slowly progressive course
5-20% have clinical remission
Survival has been measured at ˜ 50% at ˜ 10 years
Median renal survival time in MPGN, type I: 9-12 years, compared with MPGN, type II: 5-12 years
Prognosis of patients with MPGN, type III is similar to that of patients with MPGN, type I
Therapy improves survival to 60-85% at 10 years
Prognostic features of poor outcome
Sclerotic glomeruli, crescents, interstitial fibrosis, & tubular atrophy (IF/TA)
Clinical features of poor outcome
Severe nephrotic syndrome, ↑ creatinine, hypertension
Features of good outcome
Focal/mild MPGN features on biopsy, asymptomatic hematuria, subnephrotic proteinuria
˜ 30% of children with MPGN, type I have recurrence in 6 months to 1 year after transplant
˜ 40% of recurrences lead to graft failure
MACROSCOPIC FEATURES
General Features
Nephrectomy, exam at transplant, or autopsy reveals pale kidneys
± cortical yellow flecks, representing tubular lipid & interstitial foam cells
Advanced disease: Small granular kidneys ± prominent vessels
MICROSCOPIC PATHOLOGY
Histologic Features
Glomeruli
Lobular, hypercellular glomeruli with thickened capillary walls & ↑ mesangial substance
Mesangial interposition: Mesangial cells migrate into peripheral capillary walls between GBM & endothelium
Partial if only capillary wall segment involved
Circumferential if involving entire circumference of individual capillary
Produces “tram tracks” or GBM reduplication (best seen on PAS & silver) 2° to GBM synthesis
± subendothelial immune deposits (between duplicated GBMs) seen by light microscopy (PAS[+], nonargyrophilic on silver, & fuchsinophilic on trichrome)
± sclerosis; ± sclerotic mesangial nodules
Crescents in ˜ 20% of cases
± neutrophils & monocytes
Hyaline aggregates of immune complexes in capillary lumina
Type III: Burkholder variant
Combined features of type I MPGN & membranous GN
Glomerular capillary loops markedly thickened due to subendothelial & subepithelial deposits & mesangial interposition
Mesangial expansion with exudation of inflammatory cells
Type III: Anders and Strife variant
Hybrid of type II (dense deposit disease) & type I MPGN
Glomerular capillary walls have an irregular thickening that is eosinophilic, PAS(+), silver (JMS) (-)
Silver stains show frayed GBM with disrupted, “moth-eaten” appearance
Tubulointerstitium
Largely nonspecific with variable interstitial fibrosis and tubular atrophy, inflammation, & edema
Tubular resorption droplets
Interstitial foam cells
Red cell casts
Vascular changes nonspecific
ANCILLARY TESTS
Immunofluorescence
MPGN, type I
C3 in capillary walls & mesangium is classic feature
To lesser extent, IgG present followed by IgM, IgA, & C1q
Up to 25% have C3 only and would now be classified as C3 glomerulopathy
Also “lumpy-bumpy” granular C3, IgG, & early complement (C1q & C4)
“Railroad track” pattern may be seen on IF at high power
Focal C3 deposits in the TBM
MPGN, type III subtypes have similar findings
˜ 50% of cases have IgG & C3 (& less intense IgM, IgA, & C1q)
˜ 50% stain only for C3
Focal TBM C3 staining is present in ˜ 1/3 of cases
Electron Microscopy
Transmission
Large, dense deposits throughout glomerulus; primarily subendothelial but also mesangial
Produces double GBMs with mesangial interposition
GBM has a “sausage-string” or fusiform appearance
Intramembranous dense deposits in GBM reflections
Increased mesangial matrix
“Mesangialization” of capillary loops
Podocyte foot process effacement
Type III: Burkholder variant
Combined features of MPGN, type I & membranous glomerulonephritis
Subendothelial deposits & mesangial interposition
Type III: Anders and Strife variant
Hybrid of MPGN, type II (also known as dense deposit disease) & MPGN, type I
Subendothelial & intramembranous deposits
Deposits extend from GBM subendothelial to subepithelial portion, disrupting GBM lamina densa, giving a laminated, woven appearance
TBM deposits present in ˜ 1/3 of cases
Initially described using silver impregnation techniques
DIFFERENTIAL DIAGNOSIS
Systemic Lupus Erythematosus (SLE)
IF shows “full house” staining pattern
Serology(+) in SLE: ANA(+), anti-ds DNA(+)
Mixed Cryoglobulinemia
Mixed cryoglobulinemia associated with chronic hepatitis C has been associated with number of cases of MPGN, type I
Characteristic PAS(+) “pseudothrombi” can be seen in glomerular capillary loops in cryoglobulinemic GN
Clinical laboratory can help identify cryoglobulin
Infectious Diseases
History, physical, & clinical laboratory data can help favor diagnosis of infectious disease
Bacterial
Endocarditis & infected vascular shunts
Post-streptococcal acute glomerulonephritis: Elevated antistreptolysin-O (ASLO) titers
Viral: Hepatitis B & C, HIV
Protozoal: Malarial & schistosomiasis
Other: Mycoplasma, mycobacteria