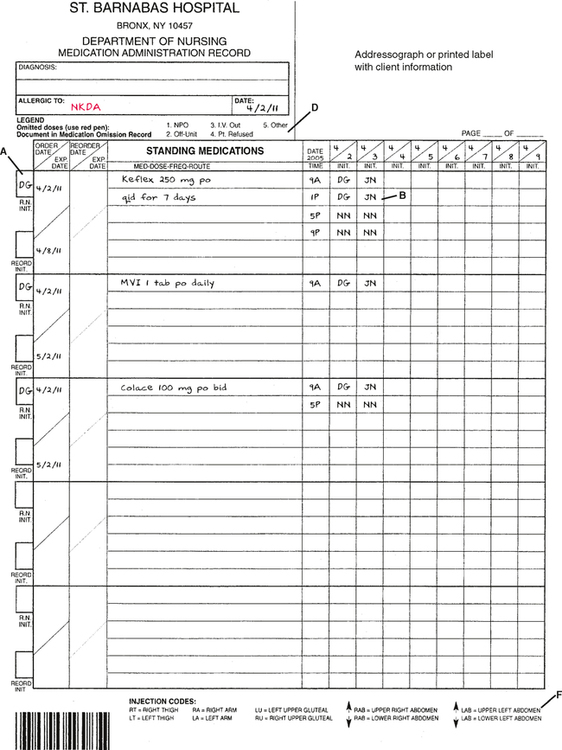
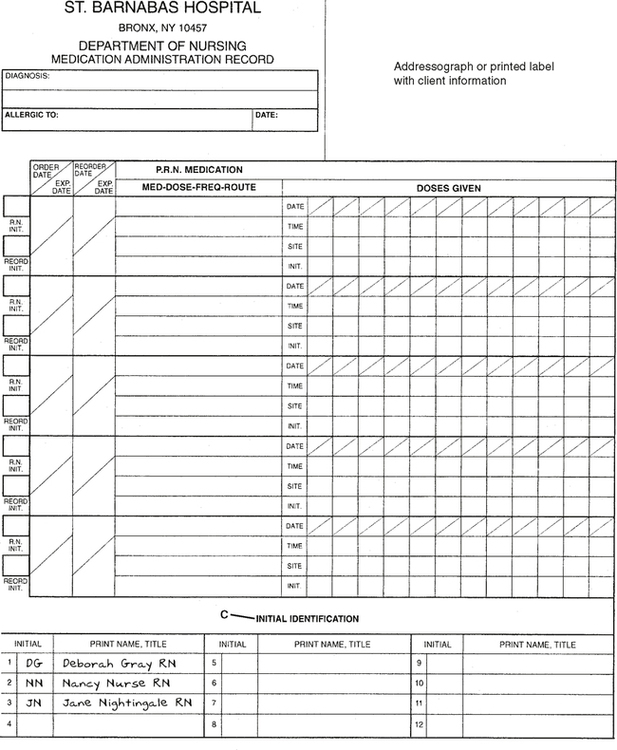
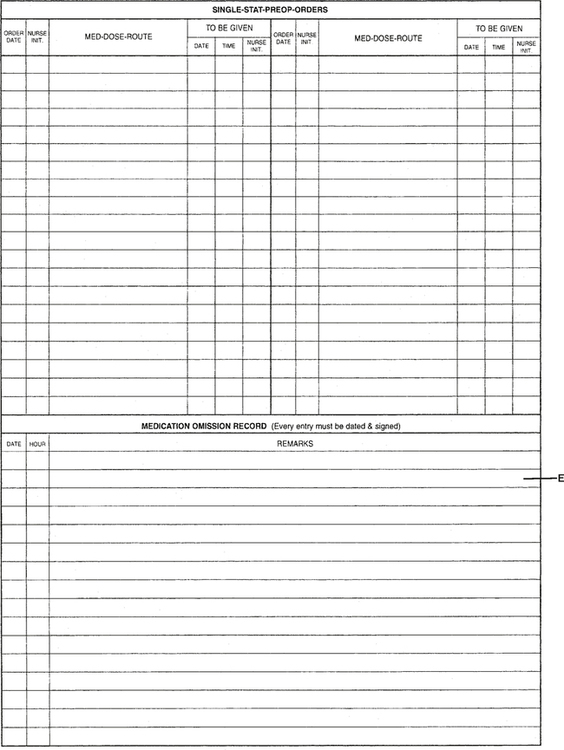
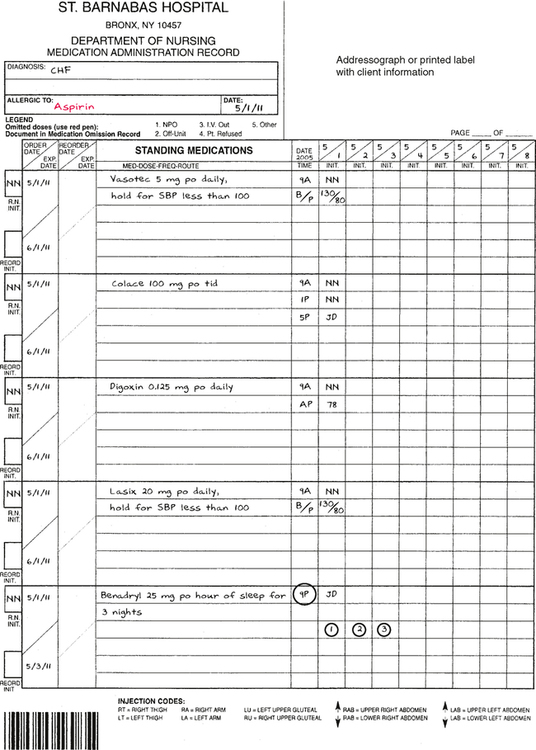
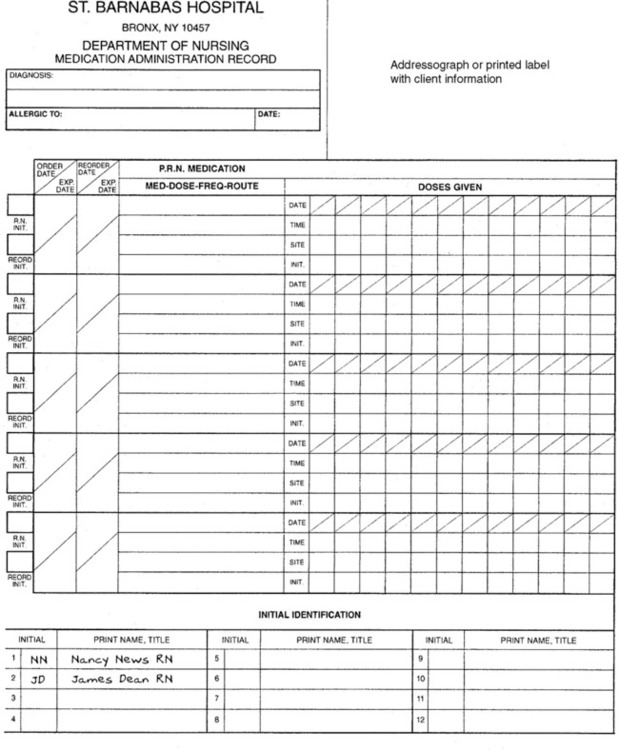
CHAPTER 12 After reviewing this chapter, you should be able to: 1. Identify the necessary information that must be transcribed to a medication administration record (MAR) 2. Read an MAR and identify medications that are given on a routine basis, including the name of the medication, the dosage, the route of administration, and the time of administration 3. Transcribe medication orders to an MAR 1. Dates. This information usually includes the date the order was written, the date the medication is to be started (if different from the order date), and when to discontinue it. 2. Medication Information. This includes the medication’s full name, the dosage, the route, and the frequency. Abbreviations used on the medication record should be standard abbreviations and follow the guidelines and restrictions of The Joint Commission, ISMP, and the health care institution. 3. Time of Administration. This will be based on the desired administration schedule stated on the order, such as t.i.d. The desired administration time is placed on the medication record and converted to time periods based on the institution’s time intervals for scheduled or routine medications. (Thus t.i.d. may mean 9 am, 1 pm, and 5 pm at one institution and 10 am, 2 pm, and 6 pm at another.) A nurse should always become familiar with the hours for medication administration designated by a specific institution. Medication times for p.r.n. and one-time dosages are recorded at the time they are administered. Abbreviations for time and frequency should adhere to The Joint Commission and ISMP guidelines. 4. Initials. Most medication records have a place for the initials of the person transcribing the medication to the MAR (Figure 12-1, A) and the person administering the medication (Figure 12-1, B). The initials are then written under the signature section to identify who gave the medication. Some forms may request the title as well as the signature of the nurse (Figure 12-1, C). The policy regarding initialing after each administration varies by institution and by charting system used. 5. Special Instructions (parameters). Any special instructions relating to a medication should be indicated on the medication record. For example, “Hold if blood pressure less than 100 systolic” or “p.r.n. for pain.” In addition to the information listed above, some medication records may include legends, as well as an area for charting to indicate when a medication is omitted or a dosage is not given. See Figure 12-1, D, for a legend of omitted doses. Other medication records may have an area where the nurse can document the reason for omission of a medication directly on the medication record (Figure 12-1, E). Other information may include injection codes so the nurse may indicate the injection site for parenteral medications (Figure 12-1, F). In cases in which no injection codes are indicated, the nurse is still expected to indicate the injection site. Space may also be allotted for charting information such as pulse and blood pressure if this information is relevant to the medication. MARs include an area for documenting medications administered. After administering the medication, the nurse or other qualified staff member must record his or her initials next to the time the drug was administered. For scheduled medications, a complete schedule is written out, and the initials are recorded next to each given time. As previously mentioned, this practice can vary by institution. With one-time dosages and p.r.n. medication, the time of administration is written and again initialed by the person administering it. The medication form has a place for the full name of each person administering medications, along with the identifying initials. This allows for immediate identification of the person’s initials if necessary. When medications are not administered, some records have notations, such as an asterisk (*), a circle, or a number corresponding to a legend on the MAR, to indicate this, or there may be an area on the back or at the bottom of the MAR for charting medications not given (see Figure 12-1, E). The type of notation used will depend on the institution. In addition to notations made on the MAR, most institutions require documentation in the proper section of the client’s chart. (Some institutions have a section designated “nurse’s notes.” At other institutions nurses may be charting on a progress note and indicate that notation “nurse’s notes”. 1. The name of the client and pertinent data related to the client 3. Time/frequency desired for administration 4. A place to indicate allergies 5. A place for date, the initials of the person who administers the medication, and a section to identify the name of the person administering the medication Unit dose is also used as part of another medication system in some institutions (e.g., a computerized unit dose medication cart). In the computerized unit-dose system, each dosage for the client is released individually and recorded automatically. This system is used for monitoring controlled substances and other items used in the unit (e.g., medications used by the unit in large volumes). The type of medication form used for this system varies from one institution to another. In some instances this system has decreased the amount of time spent transcribing orders or eliminated the need for transcription. In some institutions, however, transcription of medication orders to the MAR is still required. The prescriber’s orders are therefore written on a separate order sheet and sent to the pharmacy. Figure 12-2 illustrates the transcription of orders to the MAR.
Medication Administration Records and Drug Distribution Systems
ESSENTIAL INFORMATION ON A MEDICATION RECORD
DOCUMENTATION OF MEDICATIONS ADMINISTERED
EXPLANATION OF MEDICATION ADMINISTRATION RECORDS
MEDICATION DISTRIBUTION SYSTEMS
Unit-Dose System
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Medication Administration Records and Drug Distribution Systems