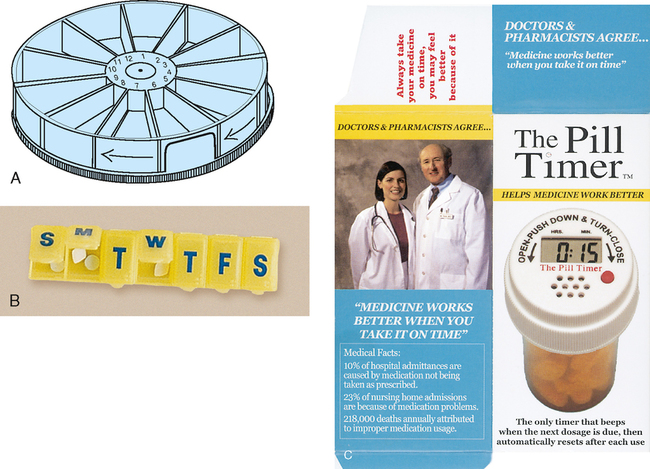
CHAPTER 10 After reviewing this chapter, you should be able to: 1. State the consequences of medication errors 2. Identify the causes of medication errors 3. Identify the role of the nurse in preventing medication errors 4. Identify the role of the Institute for Safe Medication Practices (ISMP) and The Joint Commission (TJC) in the prevention of medication errors 5. State the six “rights” of safe medication administration 6. Identify factors that influence medication dosages 7. Identify the common routes for medication administration 9. Explain the importance of critical thinking in medication administration 10. Identify important critical thinking skills necessary in medication administration 11. Discuss the importance of client teaching 12. Identify special considerations relating to the elderly and medication administration 13. Identify home care considerations in relation to medication administration • Lack of information about the client (allergies, other medications the client is taking) • Lack of information about the drug • Communication and teamwork failures • Unclear, absent, or look-alike drug labels and packages, and confusing or look-alike or sound-alike drug names • Unsafe drug standardization, storage, and distribution • Nonstandard, flawed, or unsafe medication delivery devices People are now living longer, and older people tend to use health care services more often. As with children (see Chapter 25), special consideration should be given to the client who is over 65 years of age. With the aging process come physiological changes that have a direct effect on medications and their action in the elderly individual. Aging causes the slowing down of the body’s functions. Other physiological changes include a decrease in circulation, slower absorption, slower metabolism, a decrease in excretory functions, and a decrease in the ability to respond to stress such as the stress of medications on the system. Other changes with aging include a decrease in body weight, which can affect the dosage of medications, and changes in mental status, possibly caused by the effects of physical illness or physiological changes in the neurological system that can occur with aging. These physiological changes can cause unexpected medication reactions and make the elderly person more sensitive to the effects of many medications. As a rule, the elderly client will require smaller dosages of medications (as dosage size increases, the number of adverse effects and their severity increase), and the dosages should be given farther apart to prevent accumulation of medications and toxic effects. With aging, visual and hearing problems may develop. Special attention must be given when teaching clients about their medications to help prevent medication errors. Develop a relationship with the client; building rapport and trust is important for the elderly. Take time and talk to the elderly, listen to what they say, and never assume they do not know how much or what medications they are taking. Ascertain that all instructions are written as clearly as possible, choosing fonts that are friendly to older eyes. Make sure the client has appropriate measuring devices to facilitate ease and accuracy when measuring (e.g., a dropper or measuring cup with calibrated lines to indicate small dosages [0.2 mg, 0.4 mg, etc.]). To lessen the chance of taking too much medication or forgetting a dosage, try to establish specific times compatible with the client’s routine for taking medications. Help the client to recognize pills by the name on the bottle, not by color. If the print on medications is too small for the client to read, encourage the use of a magnifying glass. Other measures might include providing a simple chart that outlines the medications to be taken, times they are to be taken, and special instructions if needed. Such a chart should be geared to the client’s visual ability and comprehension level. Encourage the elderly client to request that childproof containers not be used; some older people will have difficulty opening child-resistant containers. Recommend medication aids for the client, such as special medication containers divided into separate compartments for storing daily or weekly medication dosages. (Figure 10-1 shows examples of medication containers.) When the nurse is administering medications to a client, the six rights of medication administration should serve as guidelines. Failure to achieve any of these “rights” constitutes a medication error. The six rights (Box 10-1) should be followed when administering any medication to avoid errors and to ensure client safety.
Medication Administration
MEDICATION ERRORS
SPECIAL CONSIDERATIONS FOR THE ELDERLY
THE SIX RIGHTS OF MEDICATION ADMINISTRATION
Medication Administration