Chapter 18
Measuring population health status

Assessing health status of a population
The health of a population can be described in general terms and in relation to specific conditions. A health status profile usually considers population-level mortality rates, age, sex and cause-specific mortality rates, the prevalence and incidence of specific diseases and the prevalence of specific risk factors such as smoking or alcohol consumption. It may be compiled from routinely collected data sources or through conducting specific surveys or studies (see Chapter 17).
Summary measures of population health
Two commonly used measures of a population’s health are life expectancy at birth and infant mortality. Both are used to compare population health nationally and internationally (Figure 18a).
Life expectancy at birth is the average length of time that babies born today can expect to live if today’s age and sex-specific mortality rates applied throughout their lifetime. It, therefore, provides a useful summary of current mortality rates in a population, and is a good indicator of that population’s overall health. It cannot, however, be used to predict individual lifespan. As mortality rates are generally falling, babies born today are likely to live longer on average than today’s mortality rates currently predict. Life expectancy is reduced more by deaths in infancy and childhood than by deaths at older ages.
Healthy life expectancy (HLE) combines measures of morbidity with mortality to give an average length of time that a person in a specified population can expect to live free of disease. It provides a better means of comparison for populations with high life expectancy due to low premature mortality from common fatal diseases such as heart disease and cancer, but high levels of illness due to diseases with low mortality rates such as depression and musculoskeletal conditions. Disability-adjusted life years (DALYs) provide a similar summary measure, which includes the years of potential life lost due to premature mortality and the years of productive life lost due to disability (see Chapter 38) (www.who.int).
The fertility rate in a population is the number of live births per 1000 women of child-bearing age (usually taken as 15–44 years).
Infant mortality is a key measure reflecting the health of a population, particularly the health of pregnant women and the care given during childbirth, to newborn babies and to infants. The infant mortality rate is the number of deaths that occur in the first year of life in a specified population divided by the number of live births in that population. It is divided into several different periods (Figure 18b); deaths in each period are influenced by different factors. Perinatal mortality (stillbirths after 28 weeks’ gestation plus deaths in the first 7 days after birth per 1000 live births plus stillbirths) is heavily influenced by maternal health, care during childbirth and factors leading to premature birth. Neonatal mortality (deaths in the first 28 days after birth per 1000 live births) also reflects maternal health and care during childbirth as well as congenital conditions. Infant deaths after the neonatal period are most influenced by childhood conditions such as vaccine-preventable and diarrhoeal diseases, accidents and malnutrition. Infant mortality is generally very low in developed countries, where the main causes of death in this period are congenital conditions and accidents. In developing countries, in contrast, communicable diseases and malnutrition are the main causes of higher mortality rates.
Years of potential life lost (YPLL) is an alternative method of summarising mortality rates, which takes account of the age at which death occurs. They are usually calculated as the years of potential life lost before the age of 75 years, so that deaths occurring at younger ages, such as those from accidents, influence the summary measure more than those occurring at older ages. For example, a death at age 20 years from a road traffic accident incurs 55 YPLL compared with a death at age 70 years from a heart attack, which incurs 5 YPLL.
Survival is usually used in relation to a specified disease, rather than as a measure of population health, and is therefore most useful in monitoring the success of particular treatment strategies. It can be calculated in several ways. The crude survival rate, directly calculated, is the number of people alive at the end of a specified period of time expressed as a proportion of those who were alive at the start of the period, or from diagnosis. Corrected survival distinguishes between those dying from the specific disease of interest and those dying of other causes. Relative survival compares the survival of a particular patient or population group to a group from the general population of similar age, sex and other characteristics.
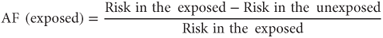
The attributable fraction (exposed) is the proportion of disease in an exposed population that would be eliminated by removing a specific causal exposure (Figure 18c):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


