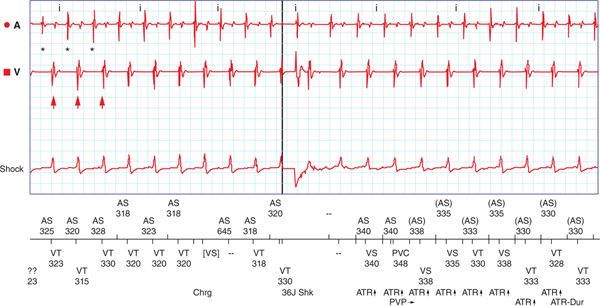
FIGURE 65-1 ICD shock delivery. After the ICD detected an arrhythmia with a higher number of ventricular (arrows) than atrial (*) depolarizations, it appropriately delivered a 35-J defibrillation.
EPIDEMIOLOGY
• Claiming the lives of more than 400 000 patients in the United States annually, sudden cardiac death is a significant public health hazard.1 The ICD improves the overall survival of many patients with left ventricular systolic function2,3 by terminating malignant arrhythmias. The survival advantage observed in clinical trials translates to a benefit in real-world populations.4
• Broadening indications and technology dissemination have led to a rise in the number of patients with ICDs, and in turn, therapies delivered by devices. The incidence of shocks varies according to patient characteristics, including the original indication for ICD placement, as well as concomitant medical therapies and device programming. In the modern therapeutic era, approximately 10% to 20% of patients experience a shock within 1 year, and 40% to 50% experience a shock within 5 years after ICD placement.5 Two in every three of these are appropriate.5
• The incidence of recurrent shocks is less understood.
ETIOLOGY AND PATHOPHYSIOLOGY
• Shocks delivered for VT or ventricular fibrillation are termed “appropriate,” while those delivered for any other reason such as supraventricular arrhythmias, noise from electromagnetic interference, or a fractured lead are called “inappropriate.”
• Appropriate shocks can occur in the setting of acute ischemia or myocardial scarring. Abrupt ischemia can trigger a number of ventricular arrhythmias, including monomorphic VT (Figure 65-2), polymorphic VT, or ventricular fibrillation. Chronic scarring and temporal dispersion of the surrounding myocardium can lead to VT whose mechanism is typically reentry.
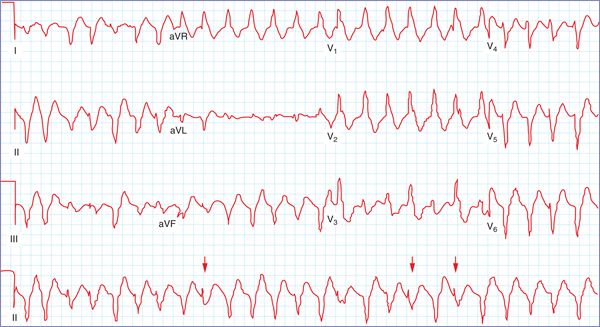
FIGURE 65-2 Monomorphic VT. Electrocardiographic features suggestive of ventricular tachycardia include atrioventricular dissociation, precordial QRS concordance, fusion beats, and capture beats. In this example, fusion beats (arrows) are readily observed in lead II.
• Appropriate shock-inducing arrhythmias are also observed in the setting of decompensated heart failure, electrolyte abnormalities, drug exposures, and genetic disorders.
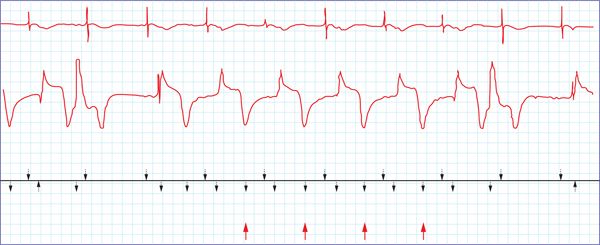
• Inappropriate shocks are most commonly caused by atrial fibrillation, supraventricular tachycardia, or sinus tachycardia (Figure 65-3A), and abnormal sensing,6 including T-wave oversensing (Figure 65-3B), double counting of the QRS complex, oversensing of diaphragmatic or skeletal myopotentials, electromagnetic interference, or a fractured lead. ICD programming is a key determinant of therapy delivery. Patients’ heart rates must exceed a detection threshold chosen by the treating physician. The duration and number of intervals at heart rates above the threshold also play a role. Programming optimization is imperfect, however, and inappropriate shocks can occur despite it. Mechanical complications related to the ICD and leads per se may also lead to shocks. Problems relating to implantation include a loose set screw, periclavicular lead placement causing a fracture, or lead dislodgment. Manufacturing defects can cause lead fractures or insulation breaks, as has been observed with the Sprint Fidelis and Riata leads respectively. Twiddler’s syndrome often occurs in the setting of psychiatric comorbidity and can cause lead dislodgement or failure.
FIGURE 65-3A Inappropriate ICD shock delivered for sinus tachycardia. Atrial depolarizations (*) preceding ventricular depolarizations (arrows) with a 1:1 ratio, QRS morphology identical to that in normal sinus rhythm, and persistence of this rhythm after a shock indicate this tachyarrhythmia was sinus tachycardia. The patient was exercising heavily at the time of the shock.
FIGURE 65-3B Inappropriate ICD shock delivered for T-wave over-sensing. Markers at the foot of the strip indicate that both QRS complexes and T waves (arrows) were sensed; this double counting led to shock delivery.
DIAGNOSIS
• When a shock is reported, an assessment is indicated. When this is performed depends on the number of shocks and the associated symptoms. If the patient does not need immediate medical attention, transtelephonic transmission is useful. Patients experiencing ≥2 shocks or significant symptoms should be assessed promptly. A careful history and physical examination is the cornerstone of any medical evaluation. A history consistent with anginal discomfort may prompt a work-up for ischemia. A history of vomiting or diarrhea may suggest an electrolyte abnormality. Review of prescribed medications may identify a culprit. Device interrogation is critical to differentiate appropriate from inappropriate therapies. VT may be differentiated from a supraventricular cause by comparing the atrial rate with the ventricular rate (see Figure 65-1). If only ventricular markers are available for analysis (such as the case in a single chamber device), a change in R-wave morphology from baseline may provide a clue.
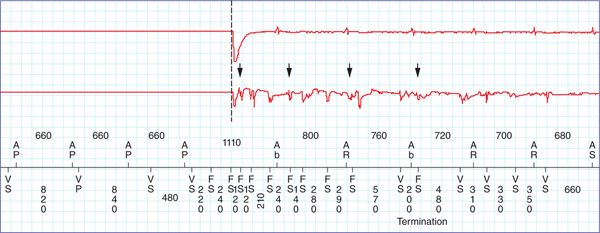
• Noise on the electrogram may indicate electromagnetic interference, a loose set screw, or a lead fracture (Figure 65-4). Software upgrades are available for various lead models that allow early detection and management of lead fractures.
FIGURE 65-4 Electrogram noise. Electrogram noise (arrows) can be caused by electromagnetic interference, a loose set screw, or a lead fracture. The patient in this example had a ventricular lead fracture.
MEDICAL MANAGEMENT
• Potentially offending medications should be stopped. Conversely, evidence-based medications should be initiated or up-titrated barring contraindications, as they reduce mortality and heart failure hospitalizations in patients with left ventricular systolic function. β-Blockers, angiotensin converting enzyme inhibitors, and mineralocorticoid receptor antagonists also favorably impact the risk of sudden death.7–9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree