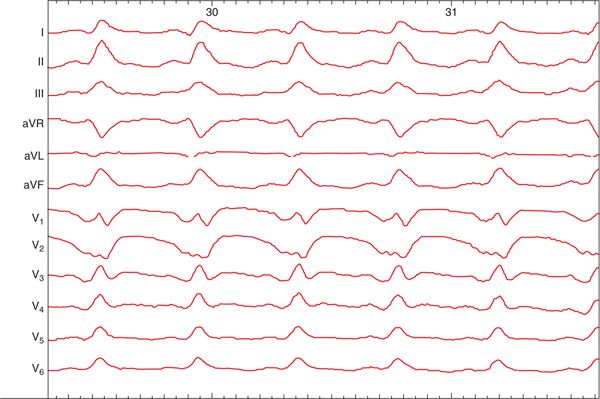
FIGURE 66-1 A 12-lead ECG of the patient’s first VT (VT1).
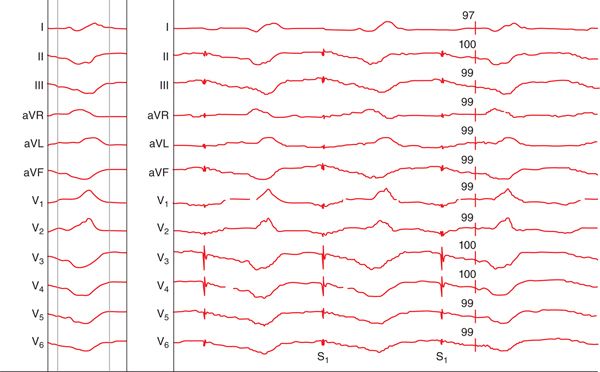
FIGURE 66-2 A 12-lead ECG of the patient’s second VT (VT2).
FIGURE 66-3A Pace map match for VT1 from the inferior apex.
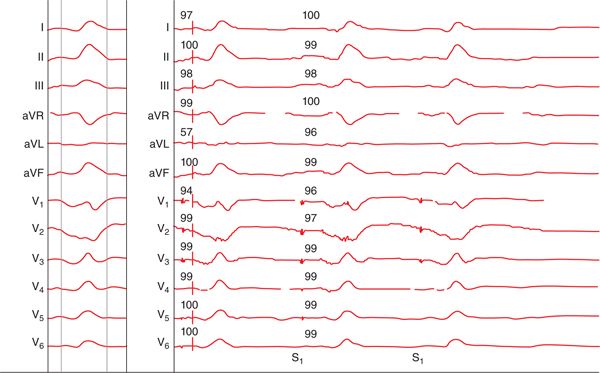
FIGURE 66-3B Pace map match for VT2 from the anterior septum.
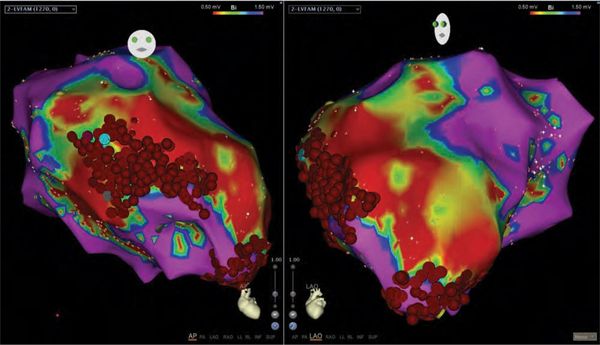
FIGURE 66-4 Activation/ablation map with straight anteroposterior view on the left and left anterior oblique view on the right. The grey dot is the dense scar. The aqua dot is the site of the pace map. The red dots are the ablation sites for the VT from the inferior apex (VT1) and from the anterior septum (VT2).
EPIDEMIOLOGY
• ICDs have been clearly demonstrated to improve the survival of patients at an increased risk of sudden cardiac death either due to prior cardiac arrest, VT, or significant left ventricular dysfunction.1–5
• A survey of ICD use in 61 countries in 2009 showed 222 407 new implants and 105 620 replacements worldwide, and the survey demonstrated a nearly 12% increase in ICD implantation in the United States between 2005 and 2009.6
• Primary prevention ICD trials demonstrated appropriate ICD shocks for VT/ventricular fibrillation (VF) in 18% of patients in Multicenter Automatic Defibrillator Implantation Trial II (MADIT-II) at 21 months7 and 22% of patients in Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) at 45 months.8
• Secondary prevention trials found appropriate ICD shocks for VT/VF in 47% of patients in the Ventricular Tachycardia Ablation in Coronary Heart Disease (VTACH) study at 23 months9 and 31% of patients in the Substrate Mapping and Ablation in Sinus Rhythm to Halt Ventricular Tachycardia (SMASH-VT) trial at 23 months.10
• Appropriate ICD shocks have serious consequences, despite their proven, life-saving efficacy.
 Long-term follow-up data from MADIT-II11 and SCD-HeFT8 found that patients have a significantly higher risk of death after appropriate ICD termination of VT or VF. Specifically, compared with patients who did not receive an appropriate ICD shock, those who did had a 3.5 times and 5.7 times higher risk of mortality in MADIT-II and SCD-HeFT, respectively.
Long-term follow-up data from MADIT-II11 and SCD-HeFT8 found that patients have a significantly higher risk of death after appropriate ICD termination of VT or VF. Specifically, compared with patients who did not receive an appropriate ICD shock, those who did had a 3.5 times and 5.7 times higher risk of mortality in MADIT-II and SCD-HeFT, respectively.
 Patients have a decline in physical functioning and mental well-being after one or more ICD shock.12
Patients have a decline in physical functioning and mental well-being after one or more ICD shock.12
DIAGNOSIS
• If the VT rate is at or above the programmed detection rate of the ICD, the VT episode is captured by the device, which makes management easier as it is often difficult to capture the VT by any other modality. Multiple VT morphologies are commonly inducible during an electrophysiology (EP) study, and the stored electrograms (EGMs) may help one identify a patient’s clinical VT.13
 Stored EGM data provide the cycle length of the clinical VT.
Stored EGM data provide the cycle length of the clinical VT.
 In 13 postinfarct patients with an ICD and with 12-lead ECGs of the clinical VT, visual inspection and computer analysis of the ICD EGMs correctly differentiated the clinical VT in 96% and 98% of the cases, respectively. This was achieved despite the fact that 67% of patients had an inducible, previously undocumented VT with a cycle length within 10% of the cycle length of the clinical VT.
In 13 postinfarct patients with an ICD and with 12-lead ECGs of the clinical VT, visual inspection and computer analysis of the ICD EGMs correctly differentiated the clinical VT in 96% and 98% of the cases, respectively. This was achieved despite the fact that 67% of patients had an inducible, previously undocumented VT with a cycle length within 10% of the cycle length of the clinical VT.
• The stored EGMs of VT episodes may also be useful in patients who are noninducible in the EP lab, which could be due to recent administration of an antiarrhythmic medication, and with normal voltage maps that preclude substrate modification.14
 A target ablation area can be identified by pacing at the tachycardia cycle length and matching the morphology of the recorded paced tachycardia to the EGM morphology.
A target ablation area can be identified by pacing at the tachycardia cycle length and matching the morphology of the recorded paced tachycardia to the EGM morphology.
MANAGEMENT
Pharmacologic Treatment of VT in ICD Patients
• Medications can reduce ICD shocks, as seen in the Optimal Pharmacological Therapy in Cardioverter Defibrillator Patients (OPTIC) trial. OPTIC was a randomized controlled trial, in which 412 patients received β-blockers alone, sotalol, or a combination of amiodarone and β-blockers.15
 Cumulative rates of shock over 1 year were 39% with β-blocker alone, 24% with sotalol, and 10% with amiodarone and a β-blocker.
Cumulative rates of shock over 1 year were 39% with β-blocker alone, 24% with sotalol, and 10% with amiodarone and a β-blocker.
 Amiodarone reduced shocks by a statistically significant amount compared with a β-blocker alone or sotalol, while sotalol had a nonstatistically significant trend toward reduction in ICD shocks compared with a β-blocker.
Amiodarone reduced shocks by a statistically significant amount compared with a β-blocker alone or sotalol, while sotalol had a nonstatistically significant trend toward reduction in ICD shocks compared with a β-blocker.
• Antiarrhythmic medications have adverse events, despite their utility in preventing tachyarrhythmias.
 In OPTIC, the discontinuation rates of amiodarone and sotalol were high even during the first year: 18% and 24%, respectively.15
In OPTIC, the discontinuation rates of amiodarone and sotalol were high even during the first year: 18% and 24%, respectively.15
 Amiodarone increases defibrillation threshold by a statistically significant amount.16
Amiodarone increases defibrillation threshold by a statistically significant amount.16
Catheter Ablation in Electrical Storm
• Four analyses of VT ablation that included ≥10 patients with electrical storm have been published, and the details of these can be found in Table 66-1.17–20
TABLE 66-1 VT Ablation in Patients with Electrical Storm*
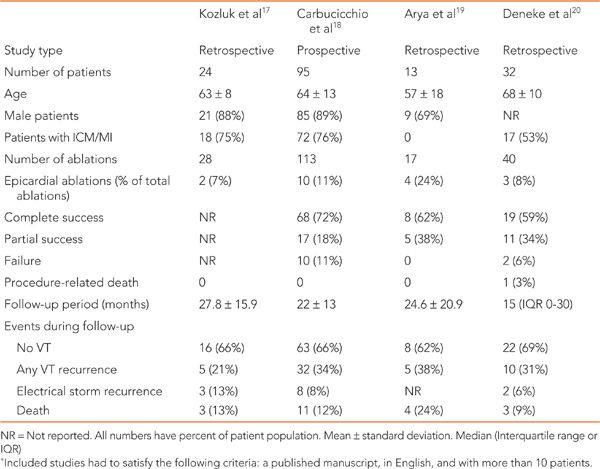
• The largest evaluation of the efficacy of VT ablation in electrical storm was a prospective study with 95 patients.18
 The patients were mostly men with ischemic cardiomyopathy.
The patients were mostly men with ischemic cardiomyopathy.
 The clinical VT was ablated in 89% of patients, and 72% of patients had no inducible VT postablation.
The clinical VT was ablated in 89% of patients, and 72% of patients had no inducible VT postablation.
 Patients were followed for a mean of 22 ± 13 months, and 66% of patients had no VT recurrence during follow-up, while only 8% of patients had recurrence of electrical storm.
Patients were followed for a mean of 22 ± 13 months, and 66% of patients had no VT recurrence during follow-up, while only 8% of patients had recurrence of electrical storm.
 There were no periprocedural deaths, but there were two transient ischemic attacks and two vascular complications.
There were no periprocedural deaths, but there were two transient ischemic attacks and two vascular complications.
• Similar rates of recurrence of VT at 62% to 69% and electrical storm at 6% to 13% were seen in the other smaller, retrospective studies.17,19,20
• The longest mean follow-up in the published studies was 28 months, and there were no long-term outcomes available on this patient population, so the durability of the effect of VT ablation remains unknown.
Catheter Ablation in Incessant Ventricular Tachycardia
• Endocardial and epicardial approaches to VT ablation have been effective in treating incessant VT with success rates of ablating the clinical VT of 90% to 94%, as shown in Table 66-2.21,22
TABLE 66-2 VT Ablation in Patients with Incessant VT*
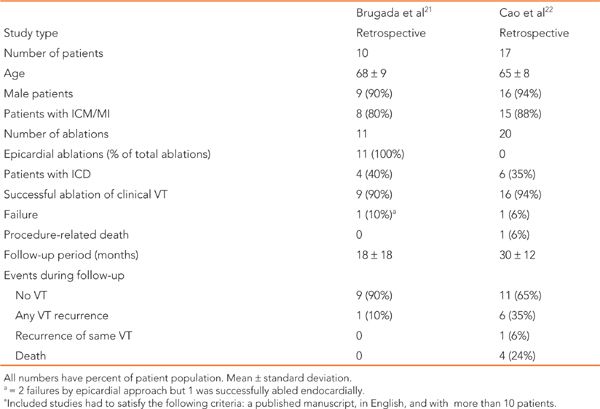
• The two studies that examined catheter ablation in incessant VT had a minority (35%-40%) of patients with an ICD.
• In these two studies, there was only one procedure-related death, resulting in a 6% periprocedural death rate in that study with 17 patients.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree