Malt Lymphoma
Scott R. Owens, MD
Key Facts
Etiology/Pathogenesis
Most gastric MALT lymphomas associated with gastritis caused by Helicobacter pylori infection
Clinical Issues
85% of all GI MALT lymphomas in stomach
Majority present with low-stage disease (I-II)
H. pylori eradication therapy 1st-line treatment for gastric MALT
Most (as many as 80% of gastric cases) respond to H. pylori eradication with regression of lymphoma
Cases with t(11;18)(q21;q21) resistant to H. pylori eradication therapy
Up to 50% of primary gastric lymphomas are MALT lymphoma
Microscopic Pathology
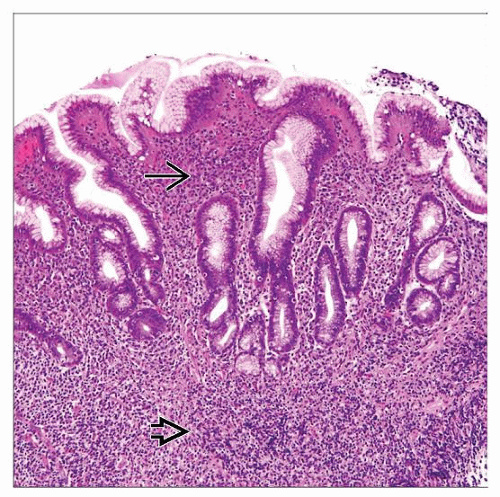
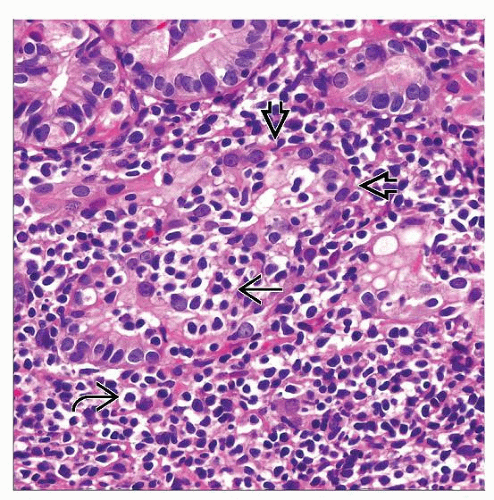
Neoplastic lymphocytes recapitulate “marginal zone” of reactive follicle
Plasmacytic differentiation seen to some extent in ˜ 1/3 of cases; occasionally predominant cell type
Lymphoepithelial lesions highly characteristic of (but not specific for) MALT lymphoma
Top Differential Diagnoses
H. pylori gastritis
Distinction of severe gastritis from early MALT lymphoma often very challenging
Diagnostic Checklist
Lymphomas composed of predominantly large cells should be diagnosed as diffuse large B-cell lymphoma (not high-grade MALT lymphoma)
TERMINOLOGY
Abbreviations
Mucosa-associated lymphoid tissue (MALT) lymphoma
Synonyms
Extranodal marginal zone lymphoma (EMZL) of MALT
Definitions
Low-grade lymphoma composed of various types of predominantly small B lymphocytes
Small- to intermediate-sized centrocyte-like cells
Monocytoid cells
Large, centroblast- or immunoblast-like cells
Plasma cells
ETIOLOGY/PATHOGENESIS
Infectious Agents
Most gastric MALT lymphomas associated with gastritis caused by Helicobacter pylori infection
H. pylori strains with CagA gene are most immunogenic
H. pylori organisms difficult to find as process evolves from gastritis to lymphoma
Serologic studies for H. pylori antibodies may be helpful
Evidence suggests association of extragastric MALT lymphomas with H. pylori as well
Immunoproliferative small intestinal disorder (IPSID)
Subtype of MALT lymphoma related to infection with Campylobacter jejuni
Antigenic Stimulation
Chronic antigen exposure → acquisition or expansion of mucosa-associated lymphoid tissue
Termed “acquired” MALT
Contains well-developed lymphoid follicles/germinal centers with surrounding lymphoplasmacytic infiltrate
In contrast to “native” MALT, such as Peyer patches in distal ileum
Continued antigenic stimulus → further expansion of B-cell population
Possible clonal expansion → lymphoma
Process thought to be driven by activated T cells
CLINICAL ISSUES
Epidemiology
Incidence
7-8% of all B-cell lymphomas
Age
Median 61 years
Gender
M:F = 1:1.2
Ethnicity
IPSID occurs in patients in subtropical and tropical locales
Site
GI tract most common site of MALT lymphoma
Up to 50% of primary gastric lymphomas are MALT lymphoma
85% of all GI MALT lymphomas in stomach
Isolated duodenal involvement uncommon
May be involved in conjunction with gastric lymphoma
Small intestinal involvement often multifocal
Distal small intestine (ileum) more frequently involved than proximal (may reflect larger native MALT population in ileum)
May involve wall circumferentially over long segments or create large, discrete mass
Obstruction uncommon as infiltrate not associated with desmoplastic stromal response
Colonic involvement relatively rare (cecum and rectum most frequent)
Other sites of extranodal involvement (e.g., elsewhere in GI tract) relatively common in gastric MALT (about 25%)
Presentation
Abdominal pain
Ulcer
Deep mass
Weight loss
Endoscopic Findings
May be difficult to distinguish from severe gastritis, especially in early cases
Cases without significant endoscopic findings difficult to follow after treatment
Mass
Ulcer
Thickened mucosal folds &/or diffuse wall thickening
Laboratory Tests
H. pylori serology
Serum protein electrophoresis
Natural History
Majority present with low-stage disease (I-II)
Bone marrow involvement uncommon at presentation
Treatment
Options, risks, complications
H. pylori eradication therapy 1st-line treatment for gastric MALT
Involves regimen of multiple medications, including antibiotics
Resolution of lymphoma can take months (up to 24 months reported)
Evidence that certain extragastric MALT lymphomas may respond to this therapy as well
More aggressive 2nd-line therapies should be reserved for truly refractory cases
Adequate time must be given for resolution
Response of lymphoma on follow-up biopsy specimens should not be anticipated for several months
IPSID may respond to broad-spectrum antibiotic therapy
Surgical approaches
Resection not usually performed
Multifocality and diffuse nature of infiltrate makes complete resection difficult
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree