38 1. At birth and in very young boys, the normal foreskin is non-retractile because of glanulo-preputial adhesions but the preputial orifice is unscarred and pliant. This normal appearance is clearly distinguishable from a pathological phimosis (tight non-retractile foreskin). 2. As boys mature, the glanulo-preputial adhesions separate and the foreskin becomes retractile. 3. Pathological phimosis in boys is usually caused by lichen sclerosus. The preputial orifice is pale, scarred, and non-pliant. This condition affects less than 1% of boys, peaks in incidence at age 11 and is rarely encountered before the age of 5. The condition is the main medical indication for paediatric circumcision. Recurrent balano-posthitis is a further relative indication. 4. In adults, the medical indications for circumcision are phimosis, paraphimosis (inability to reduce a retracted foreskin over the glans penis to its naturally occurring position), recurrent balano-posthitis and suspected or established penile cancer. Some men with recurrent cracking or tearing of the foreskin or frenulum and certain skin conditions refractory to medical treatment (e.g. genital warts) also benefit from circumcision. 5. In many cultures, circumcision is performed for ritual or religious reasons. 6. Patients and parents seeking circumcision should be counselled fully about the short and long-term risks and benefits of the procedure. 7. Consent should include the risk of bleeding and superficial infection as well as alteration in sexual sensation. 8. In addition to surgical circumcision, there are several non-surgical methods using a variety of clamps or constriction devices which aim to cause ischaemic necrosis of the foreskin. 1. Adult circumcisions can be performed under general anaesthesia or with a local anaesthetic penile ring block using a combination of short-acting (lidocaine) and long-acting (bupivicaine) local anaesthetics. Calculate the dose according to the patient’s body weight and never use adrenaline. Inject a good bolus just under the pubic symphysis in the midline where the dorsal nerves pass. Inject further anaesthetic around the base of the penis in a ring. 2. Perform paediatric circumcision under general anaesthesia. 1. Firstly, retract the foreskin to clean the glans. If the phimosis is severe, this can be done by placing an artery clip through the preputial opening and opening the clip to widen the orifice. If this is not possible, the tight band can be incised with tissue scissors. 2. Once the foreskin is retracted, use a probe to release the adhesions from the glans and define the coronal margin. Use antiseptic wash to thoroughly clean the glans and remove any inspissated smegma. 3. Replace the foreskin and apply two straight artery forceps side by side in the midline on the dorsal surface of the foreskin (Fig. 38.1A). Divide between these two forceps with scissors, taking care not to cut the glans with the inner blade of the scissors (Fig. 38.1B). Continue the incision until about 0.5 cm short of the corona (depending on the age of the child or the size of the penis), which leaves a cuff of tissue below the corona (Fig. 38.1C). 4. From the apex of this incision cut laterally around the base of the glans creating an even cuff of tissue all the way round to the frenulum on one side and then the other (Fig. 38.1D). Ensure that both the inner and outer layers of the foreskin are cut together to give a good cosmetic outcome. 5. Use bipolar diathermy to achieve haemostasis. The small artery of the frenulum may need to be tied. 6. Reconstruct the frenulum with a fine absorbable suture (Fig. 38.1E) and leave one end long to act as a stay. Place the second suture on the dorsal side in the midline and again create a stay stitch. The penis can be manipulated between the two stay sutures and the two layers of the foreskin can be opposed with fine absorbable interrupted sutures (38.1F). 1. With a pen, mark the line of incision just above the level of the corona on the foreskin. On the ventral aspect of the penis follow the natural tapering of the corona. 2. Use a blade to incise the skin over your marked line. Take care not to sever the large veins that lie just beneath the skin. Divide the veins between clips and tie them. 3. Retract the foreskin to expose the glans. If the phimosis is very tight, use scissors to make an incision through the dorsum of the foreskin to allow retraction. Then make a second circumferential incision with the knife on the inside surface of the retracted foreskin about 0.5 cm from the corona. 4. Excise the skin between the two circumferential incisions. 5. Apply careful haemostasis with bipolar diathermy and ties where appropriate. 6. Approximate the two cleanly cut skin edges with interrupted fine absorbable sutures as described above. 1. A tight frenulum may present clinically as a non-retractile foreskin or pain on retraction, painful erections or pain on intercourse. 2. A tight frenulum may be congenital or it may result from scarring. 3. Obtain consent including possible alteration in sexual sensation, persistent symptoms and the possible need for subsequent circumcision. 1. Perform this procedure under general anaesthesia or under local anaesthesia with a penile block. 2. Retract the foreskin fully and this will usually define the tight band of the frenulum. 3. Incise the frenulum transversely over the tight band, releasing the subcutaneous tissues as well as the skin. Do not incise too deeply as this may result in a urethral injury. 4. Use bipolar diathermy to achieve haemostasis. 5. Close the incision longitudinally with a fine absorbable suture. This lengthens the frenulum by 0.5–1 cm. 1. A hydrocele is an abnormal collection of fluid contained within the tunica vaginalis and usually surrounds the testis. 2. The testis cannot be palpated separately from the hydrocele collection. 3. Undertake surgical repair if the hydrocele produces troublesome symptoms. Asymptomatic or minimally troublesome hydroceles are best left alone. 4. Three commonly practised surgical repairs are the Lord’s plication, the Jaboulay procedure and hydrocele excision. There is minimal dissection of the hydrocele sac with Lord’s plication, resulting in a relatively bloodless procedure. This technique works well with thin-walled hydroceles that are not too large. Jaboulay eversion and excision of the hydrocele sac require more dissection of the sac, with increased opportunities for bleeding but are more suited to thick-walled hydroceles. 1. Check the imaging and mark the side to be operated on. 2. Incise either along the midline raphe or use a transverse scrotal incision, avoiding small vessels in the skin. 3. Use a hand-held diathermy point to deepen the incision through the dartos layer. 4. For Lord’s procedure, incise the tunica to drain the hydrocele fluid and then extend the incision in the tunica using scissors. Make the incision large enough to deliver the testis. Note that in Lord’s procedure the hydrocele sac is not dissected from the dartos layer. 5. To perform the plication, use interrupted absorbable sutures to gather together the tunica in several small bites, starting from the cut edge and working towards the testis. Avoid placing the suture through the epididymis. After all the sutures have been placed, the tunica vaginalis appears bunched around the testis, thus obliterating the hydrocele sac (Fig. 38.2). 6. For a Jaboulay procedure, the hydrocele sac is dissected from the overlying dartos and the hydrocele and testis delivered through the incision. 7. Incise the tunica vaginalis, evert it behind the testis and re-approximate the edges around the cord and epididymis posterior to the testis, using a continuous absorbable suture. 8. Alternatively, excise the tunica vaginalis close to the testicle and achieve haemostasis by running a fine continuous absorbable suture around the cut edge. 9. Before returning the testis to the scrotum, apply meticulous haemostasis using diathermy or ties where appropriate. 10. Close the dartos using a continuous absorbable suture, taking large bites of this muscle layer to aid haemostasis. 11. Close the scrotal skin with absorbable interrupted mattress sutures. 12. A scrotal support minimizes swelling and reduces the risk of scrotal haematoma formation. 1. Excise epididymal (Greek: epi = upon + didymos = twin; upon the testes) cysts only when they become uncomfortably large. 2. Removal of epididymal cysts is relatively contraindicated in young males as it may cause epididymal damage leading to reduced fertility. 3. The condition is multiple, so warn patients that recurrent cysts are likely. 1. Check any imaging and mark the side to be operated on. 2. Incise the scrotal skin as described for excision of a hydrocele sac. Deepen the incision through the scrotal layers using a handheld diathermy point or knife. 3. Deliver the testis along with its appendages, including the cysts. Remember that cysts are often multiple and commonly occur in the upper pole of the epididymis. 4. Combine blunt and scissor dissection. Hold the testis with one hand, or have an assistant hold it, while you clean off all the adventitial tissue surrounding the cyst. 5. With scissors, completely excise the cyst or else de-roof it by cutting off the whole protruding surface. 6. If there are very many cysts, excise that part of the epididymis bearing them. 7. Oversew the raw area left following this, using fine absorbable sutures. 8. Return the testis to the scrotum and close as described for hydroceles.
Male genitalia
CIRCUMCISION
Appraise
Prepare
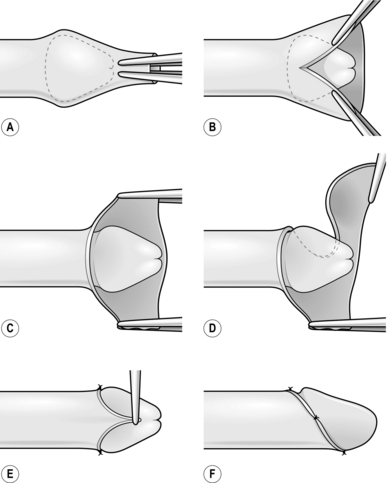
Action
ADULT CIRCUMCISION
Action
FRENULOPLASTY
Appraise
Action
HYDROCELE REPAIR
Appraise
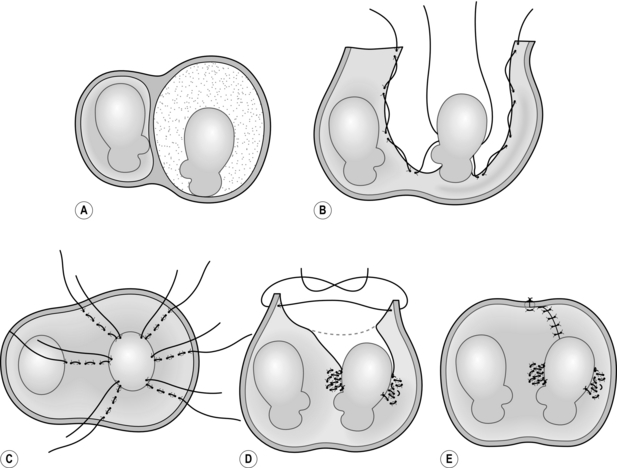
Action
EXCISION OF EPIDIDYMAL CYSTS
Appraise
Action
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Male genitalia