Lymphomatoid Papulosis
Aaron Auerbach, MD, PhD
Key Facts
Terminology
One of the CD30(+) T-cell lymphoproliferative disorders
Recurrent lymphoproliferative cutaneous disorder
Disorder with self-healing lesions that regress without treatment and have atypical CD30(+) T cells in polymorphous background
Clinical Issues
Papules or nodules at different stages of development that regress
20% have LyP-associated malignant lymphoma
Excellent prognosis
Microscopic Pathology
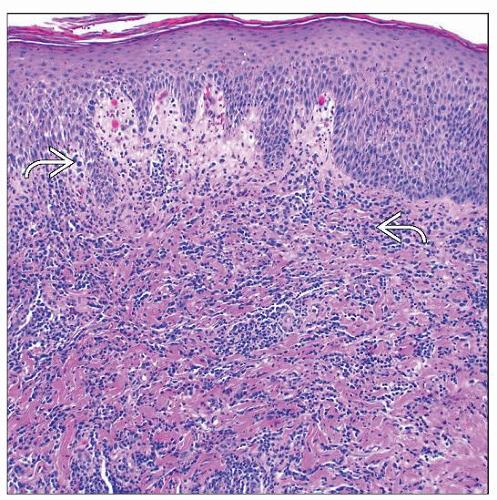
Often wedge-shaped infiltrate; large atypical T cells
Polymorphous background infiltrate
4 types: A, B, C, and D
Ancillary Tests
CD3(+), CD30(+), CD4(+), CD8(−), cytotoxic markers(+)
t(2;5)(p23;q35) negative
Clonal T-cell receptor gene rearrangement in 40%
Top Differential Diagnoses
Primary and systemic anaplastic large cell lymphoma
Differentiated from LyP based on morphology and clinical course
Reactive conditions
Infection and drug reaction can mimic LyP by showing clusters of atypical CD30(+) cells
Mycosis fungoides
Similar to type B LyP with epidermotropism
 In this clinical photograph of LyP, there are papules around the buttocks and lower legs at different stages of evolution. (Courtesy R. Willemze, MD.) |
TERMINOLOGY
Abbreviations
Lymphomatoid papulosis (LyP)
Definitions
Recurrent, self-healing cutaneous lesions composed of CD30(+) atypical T cells in polymorphous inflammatory background
One of the CD30(+) T-cell lymphoproliferative disorders (LyP, primary cutaneous anaplastic large cell lymphoma [C-ALCL], and borderline cases)
ETIOLOGY/PATHOGENESIS
Idiopathic
Viral infection, chronic antigenic stimulation, and immunosuppression have all been implicated as factors in some cases
CLINICAL ISSUES
Epidemiology
Incidence
0.1-0.2 cases per 100,000
Age
Mostly adults (30s to 50s), median age 45, less common in children
Gender
Male:female = 3:1
Site
Disease usually confined to skin
Common on trunk and extremities
Presentation
Multiple erythematous papules or nodules
± ulceration
Lesions at different stages of development
New lesions simultaneously occur at multiple anatomic sites
New lesions develop as old lesions regress
May form vesicular, crusted, or hemorrhagic lesions
Natural History
Lesions spontaneously heal with scarring
Individual skin lesions regress within 3-12 weeks
Duration of disease
Waxing/waning clinical course; may persist for up to 40 years
LyP-associated malignant lymphoma
Up to 20% of patients with LyP have another lymphoma
LyP may precede, proceed, or occur simultaneously with associated malignant lymphoma
Mycosis fungoides (MF), ALCL, Hodgkin lymphoma most common
Treatment
Adjuvant therapy
No specific treatment for most patients other than follow-up to monitor changes in skin lesions
Sometimes low-dose methotrexate ± irradiation and psoralen ultraviolet A
Prognosis
Excellent
˜ 100% 5-year survival
2% of associated lymphomas lead to death
MICROSCOPIC PATHOLOGY
Histologic Features
Dermal infiltrate, often wedge-shaped or band-like, of medium- to large-sized T cells
Sometimes angiocentric
Folliculotropic if CD30(+) cells around hair follicles
Epidermis may show ulceration, hyperkeratosis, and parakeratosis
Variable histology with 4 subtypes (A, B, C, D) representing spectrum of disease
Type A (mixed infiltrate)
Few scattered large atypical Reed-Sternberg-like or multinucleated cells
Abundant reactive polymorphous inflammatory cells
Type B (mycosis fungoides-like)
Epidermotropism of small T cells showing cerebriform nuclei
Only 10% of LyP cases
Cannot be separated from MF by histology or immunohistochemistry
Type B LyP spontaneously regresses, unlike MF
Type C (ALCL-like)
Monotonous sheets of large atypical cells
Scant polymorphous background infiltrate
Cannot be separated from ALCL by histology or immunohistochemistry
Type D (cytotoxic T-cell variant)
Marked epidermotropism and CD8(+)
Polymorphous background infiltrate
Histiocytes, neutrophils, eosinophils, and lymphocytes
Biopsy may show overlapping features of type A, B, or C
ANCILLARY TESTS
Immunohistochemistry
T-cell antigens expressed: CD2(+), CD3(+), CD5(+), CD7(+)
± loss of T-cell antigens (CD7 most common)
CD30(+) necessary for diagnosis of type A and type C
CD30 often (−) in type B
ALK(−), EMA(−)
Usually CD4(+), CD8(−), rarely CD8(+) cases (type D)
Sometimes (+) for CD15, CD56 (10%), CD25, MUM1, TRAF, and Bcl-2
Cytotoxic markers (+) (TIA-1, granzyme-B, perforin)
Cytogenetics
No specific abnormalities
In Situ Hybridization
t(2;5)(p23;q35) negative