Lymphomatoid Granulomatosis
Key Facts
Terminology
Angiocentric lymphoproliferative disorder composed of Epstein-Barr-infected B cells admixed with reactive T cells
Clinical Issues
Cough
Dyspnea
Microscopic Pathology
Sheets of mixed, polymorphous atypical lymphoreticular infiltrates with destruction of lung parenchyma and extensive areas of necrosis
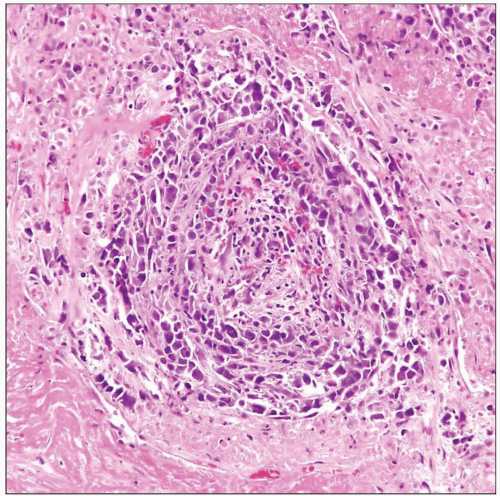
Most salient feature is prominent angiocentricity of atypical lymphoid cells, with concentric arrangement of lymphoid cells replacing the intima and media
Atypical lymphoid cells may be large and mononuclear or binucleated, resembling Reed-Sternberg cells
LYG is subdivided into 3 grades based on number of large, EBV-positive cells in the infiltrate
Atypical lymphoid cells may be large, mononuclear or binucleated, resembling Reed-Sternberg cells
Ancillary Tests
Bulk of infiltrate is composed of reactive small CD2(+), CD3(+), CD4(+) T-helper lymphocytes
Larger, atypical cells are positive for CD20 and CD79a
Large, atypical cells are positive for EBV-latent membrane protein
Large atypical cells react positively for EBV-encoded ribonucleotides (EBER) by in situ hybridization technique
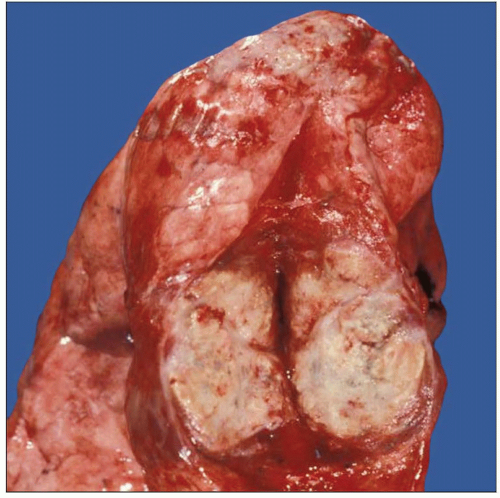 Cut surface of the lung in a patient with lymphomatoid granulomatosis shows a well-circumscribed, gray-white fleshy nodule with areas of necrosis. |
TERMINOLOGY
Abbreviations
Lymphomatoid granulomatosis (LYG)
Synonyms
Angiocentric immunoproliferative lesion
Definitions
Angiocentric lymphoproliferative disorder composed of Epstein-Barr-infected B cells admixed with reactive T cells
ETIOLOGY/PATHOGENESIS
Pathogenesis
Epstein-Barr-driven lymphoproliferative disorder arising in background of immune deficiency
CLINICAL ISSUES
Epidemiology
Incidence
Rare disorder
Most commonly occurs in immunosuppressed patients
Seen in association with AIDS, transplants, or Wiskott-Aldrich syndrome
Age
Most common in middle-aged adults
Can also occur in young adults and children
Presentation
Cough
Dyspnea
Laboratory Tests
Impaired in vitro responsiveness to mitogens
Diminished humoral and cell-mediated responsiveness to Epstein-Barr virus
Decrease in total T cells, CD4 and CD8 lymphocytes
Natural History
Disease is most often confined to lung but can involve other organs, including
Skin
Central nervous system
Kidney
Some cases may progress to diffuse large B-cell lymphoma
LYG is associated with up to 70% mortality, but some cases may regress spontaneously
Treatment
Adjuvant therapy
Combination chemotherapy and corticosteroids
Rituximab
Antiviral agents
Interferon has contributed to remission in some patients
IMAGE FINDINGS
Radiographic Findings
Multiple bilateral and peripheral nodular opacities ± cavitation
May also present with diffuse reticulonodular infiltrates or with a solitary mass
MACROSCOPIC FEATURES
General Features
Well-circumscribed tumor mass with homogeneous gray-white cut section
Lesions frequently contain central areas of necrosis
MICROSCOPIC PATHOLOGY
Histologic Features
Sheets of mixed, polymorphous atypical lymphoreticular infiltrates with destruction of lung parenchyma and extensive areas of necrosis
Most salient feature is prominent angiocentricity of atypical lymphoid cells
Transmural infiltration of small and medium-sized vessels by atypical lymphocytes
Concentric arrangement of lymphoid cells replacing media and intima of vessels
Cytologic Features
Infiltrate is polymorphous and contains abundant small lymphocytes, plasma cells, histiocytes, and scattered atypical lymphoid cells
Atypical lymphoid cells may be large and mononuclear or binucleated, resembling Reed-Sternberg cells
LYG is subdivided into 3 grades based on number of large, EBV-positive cells in the infiltrate
Grade I: Small lymphocytes predominate, and large, EBV-positive B-lymphocytes are scarce (< 5% of infiltrate)
Grade II: Large, EBV-positive B-lymphocytes are increased and account for 5-20% of lymphoid infiltrate
Grade III: Large, EBV-positive B-lymphocytes predominate, and lesion resembles a diffuse large-cell lymphoma
ANCILLARY TESTS
Immunohistochemistry
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree