Lymphocytic Colitis
Julianne K. Purdy, MD
Key Facts
Clinical Issues
Middle-aged to elderly individuals
Less pronounced female predominance than in collagenous colitis (CC); M:F = 1:1-5.7
Chronic nonbloody diarrhea
More mild clinical course than CC
Macroscopic Features
Normal colonoscopy
Microscopic Pathology
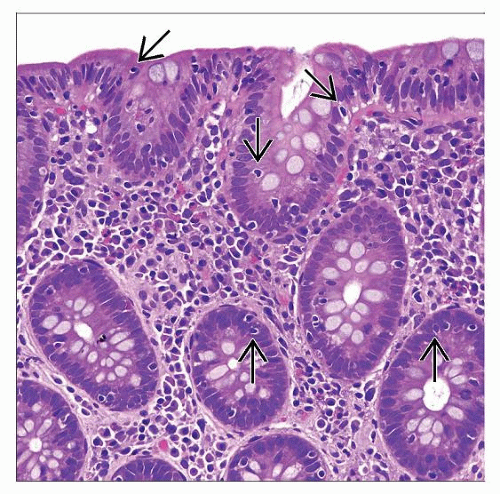
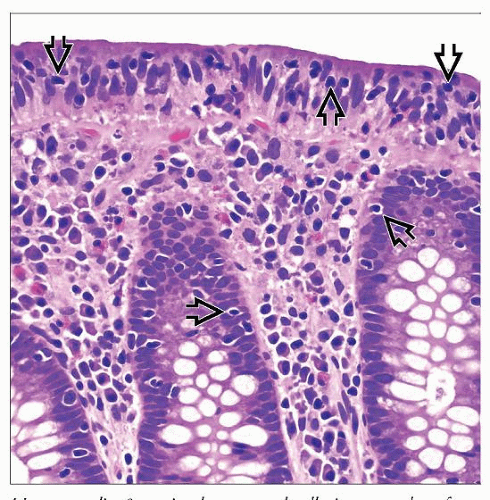
Increased surface intraepithelial lymphocytes (usually > 15-20 IELs/100 epithelial cells)
Increased mononuclear inflammation in lamina propria (mainly plasma cells, fewer lymphocytes)
Surface epithelial damage: Flattening, loss of mucin
No increased subepithelial collagen
Normal crypt size, shape, architecture
Focal IBD-like changes possible
Top Differential Diagnoses
Collagenous colitis
Increased subepithelial collagen
More chronic inflammation in lamina propria; eosinophils
Surface epithelial sloughing
Inflammatory bowel disease
Erosion/ulceration, increased intraepithelial PMNs
Crypt architectural distortion, basal plasmacytosis, marked cryptitis, crypt abscesses
Infectious colitis: Brainerd diarrhea
Lesser degree of intraepithelial lymphocytosis and surface epithelial degeneration
TERMINOLOGY
Abbreviations
Lymphocytic colitis (LC)
Definitions
Form of microscopic colitis with markedly increased intraepithelial lymphocytes (IELs), no increased subepithelial collagen, and normal colonoscopy
ETIOLOGY/PATHOGENESIS
Immunologic Reaction to Luminal Antigen
Infection
LC patients may have sudden single attack of diarrhea and respond to antibiotics
Seasonal onset (summer and fall)
Resemblance to Brainerd diarrhea
Outbreaks of watery diarrhea described in Brainerd, Minnesota
No microorganism ever isolated
Fewer surface IELs than LC; no surface damage
Association with C. jejuni infection
Association with E. coli
Recently identified/reclassified E. coli associated chronic diarrhea
Bacilli adherent to colonic mucosa: Significant correlation with epithelial damage, lamina propria infiltrate
E. coli(+) stool cultures significantly more frequent in LC patients
Food antigen (i.e., gluten): LC-like changes in celiac disease patients given gluten enema
Drugs
Most clear causal relation: Ticlopidine, flutamide
Others: Carbamazepine, cimetidine, ranitidine, lansoprazole, gold salts, paroxetine, sertraline
NSAIDs: 30-79% of LC patients; no direct causal link
Autoimmune Mechanism
Autoimmune disease: 20-60% of LC patients
Celiac disease, thyroid disorders, diabetes, psoriasis, rheumatoid arthritis most common
Celiac disease: 6-27% of LC patients
Common toxic luminal agent (besides gluten) → sensitization of both small bowel and colon
May be concurrent diseases
Genetic Predisposition
HLA data inconclusive
Familial cases: Possibly environmentally related
Family history of intestinal inflammatory disease
Crohn disease, UC, collagenous colitis, celiac disease: 12% of LC patients
Crohn disease or UC: 2-7% of patients
Common abnormality could predispose to LC and inflammatory bowel disease
Unknown Etiology
Most cases idiopathic
Likely various causes, linked to abnormally functioning immune system
CLINICAL ISSUES
Epidemiology
Incidence
3.1-5.7/100,000 people/year (USA, Europe)
Prevalence up to 63.7/100,000 (USA)
Age
Median age at diagnosis is 59-67 years
Gender
M:F = 1:1-5.7
Presentation
Chronic nonbloody diarrhea
May be nocturnal
Onset may be sudden and can mimic infection
Chronic and intermittent; less likely continuous
Histologic LC without diarrhea: 4% of cases
Mild intermittent crampy abdominal pain
Weight loss, fatigue, bloating, tenesmus, fecal incontinence, nausea
Symptoms milder and less likely to persist than in collagenous colitis (CC)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree