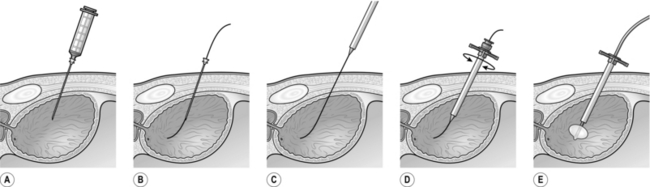
37 1. Suprapubic catheterization is indicated in both emergency and elective settings. A suprapubic catheter (SPC) may be required to drain a bladder in acute urinary retention when urethral catheterization is not possible, e.g. in the presence of a urethral stricture, or to divert urine following injury to the lower urinary tract such as from a pelvic fracture. 2. An SPC may also be used to divert urine following complex reconstructive urological surgery. 3. SPCs are the preferred option for long-term catheterization. By bringing out the catheter through a clean part of the anatomy it is easier to maintain hygiene around the catheter site. Changing an SPC is a clean and technically easy procedure. The risk of infection is reduced, although not completely eliminated. An SPC leaves the genitals free for sexual activity. 1. The bladder lies in the anterior part of the pelvic cavity behind the fat -filled retropubic space. As the bladder fills, it rises above the pubic crests and comes into contact with the lower part of the anterior abdominal wall. 2. The distended bladder intervenes between the parietal peritoneum and the abdominal wall and access can be gained without breaching the peritoneum. 3. The layers of the anterior abdominal wall are firstly the skin and subcutaneous fat. Scarpa’s fascia is the next layer. It is well defined and can be thick in obese patients. Deep to Scarpa’s fascia, in the midline, below the level of the umbilicus, the rectus sheath forms a single fibrous layer which passes anterior to the rectus abdominis muscles. The posterior surface of the rectus muscles is in direct contact with the transversalis fascia, beneath which is the extra-peritoneal fat. 1. There are three types of suprapubic catheter – one where the catheter is introduced over its own needle (the Bonanno™ catheter); the second relies on a Seldinger technique of placing a guide-wire, dilating the track and then introducing the catheter; the third type is introduced via a trocar and cannula placed blindly. 2. The Bonanno™ catheter (BD Biosciences) is a fine-bore catheter tube that can be used as a temporary method of draining the bladder. Due to the narrow calibre of the catheter it is prone to blocking and is not suitable for medium or long-term use. 3. Foley balloon catheters are preferred for suprapubic drainage and are generally available in kits for insertion. Prepare the patient’s abdomen in the supine position. Place the drapes to ensure that the midline of the abdomen is identifiable. 4. Locate the site for insertion, two finger-widths above the pubic symphysis in the midline. Use ultrasound to localize the bladder, if available. Infuse local anaesthetic into the skin and the subcutaneous tissues. Continue to advance the needle through all the layers of the anterior abdominal wall until urine is aspirated. 5. Introduction of a suprapubic catheter can only be safely performed following aspiration of urine. 6. Place a 1-cm incision at the site of injection using a blade and deepen it through the subcutaneous fat. 7. Insertion of an SPC using the Seldinger method is considered to be the safest method due to the higher degree of control and accuracy of placement. 8. Attach a long 18-gauge needle to a syringe for deep local anaesthetic infiltration and aspiration of urine from the bladder (Fig 37.1A). Once aspiration is confirmed, detach the syringe leaving the needle in place with its tip still in the bladder. Insert the floppy tip of a guide-wire through the long needle into the bladder (Fig 37.1B). Remove the needle over the guide-wire. Feed the stiff end of the guide-wire through the aperture in the tip of the trocar (Fig 37.1C) and advance the trocar along the guide-wire into the bladder (Fig 37.1D). Remove the trocar leaving the sheath in situ. Introduce a Foley catheter through the sheath and inflate the balloon (Fig 37.1E). 9. If using a blind trocar, push the trocar in its sheath through the skin incision angled at 90o to the skin. Apply constant pressure with rotational movements as you advance the trocar. A sudden loss of resistance will indicate penetration of the rectus sheath. This does not indicate access to the bladder. The trocar will need to be advanced further to enter the bladder. 10. Confirm access to the bladder by withdrawing the trocar from its sheath to observe a flow of urine. If no urine is seen, replace the trocar in the sheath and advance further until urine is obtained. Insert the catheter quickly through the sheath into the bladder and inflate the balloon. Remove the sheath and secure the catheter with a non-absorbable suture. 11. Where suprapubic catheterization is required electively for long-term catheterization, perform this under direct vision by filling the bladder with a flexible or rigid cystoscope. The cystoscope is used to watch the safe placement of the instruments from within the bladder. 1. There are very few indications for you, as a general surgeon, to cystoscope a patient. 2. However, you may be forced to pass an instrument, usually a rigid one, in order to relieve clot retention. The procedure is very similar to passing a metal urethral dilator (see below). 3. If you are a junior doctor working on a urological firm you will be expected to undertake this procedure safely as a core skill. 1. Use general anaesthesia when possible. 2. Place the patient in the lithotomy position. 3. Clean and appropriately drape the patient. 4. Check the cystoscope for lighting and irrigation. 5. Insert the lubricated cystoscope under direct vision, using a 0o or 12o rod lens telescope, with the irrigation running. In a male patient, stretch the penis and hold it straight at an angle of about 45o to the horizontal. Slowly advance the scope, visualizing the whole urethra. As you approach the external sphincter lower your hands so the scope is approaching the horizontal. Carefully advance the scope through the sphincter. You will see the verumontanum (a small raised structure in the 6 o’clock position). At this point, do not advance any further; drop your hands further so the scope is now pointing upwards and you can see the two lobes of the prostate. When the scope is pointing upwards at about 45o, advance the scope into the bladder. 6. There is no justification for passing the cystoscope blindly. This is particularly important immediately following prostatectomy, when ‘blind’ passage of the cystoscope can be extremely difficult and its tip may undermine the trigone. 7. Inspect the bladder using a methodical approach to ensure that it is inspected in its entirety. You may need to exchange the telescope for a 30o or 70o lens for complete inspection. 8. When the bladder is full of clot, it is often necessary to pass the larger 27 F resectoscope sheath in order to evacuate the clots effectively. Use a visual obturator to insert the resectoscope under vision using the principles described above for passing the cystoscope. If the visual obturator is not available and you have to insert the resectoscope sheath ‘blind’, obtain a preliminary view of the urethral anatomy with the cystoscope to help you know where you are going. Clots can be evacuated from the bladder using an Ellik’s evacuator. 1. Urethral strictures commonly cause symptoms of bladder outflow obstruction and are the most common cause of urinary obstruction in young and middle aged men. 2. Any injury to the epithelium lining the urethra or to the underlying corpus spongiosum which results in healing by scar formation may cause a urethral stricture. 3. The aetiology may be infective (Chlamydia, gonococcal), traumatic (usually blunt or iatrogenic), inflammatory (e.g. lichen sclerosus et atrophicus), ischaemic (secondary to distraction injury) or idiopathic. 4. Traumatic strictures may occur after straddle injuries, kicks to the perineum or pelvic fractures. Iatrogenic trauma is a common aetiology and any form of urethral instrumentation resulting in urethral epithelial damage may subsequently result in stricture formation. This can range from minor instrumentation such as urethral catheterization to bladder neck strictures resulting from transurethral resection of the prostate. 5. Strictures have a high recurrence rate following endoscopic treatment. Recurrence is more common with longer and denser strictures. 1. Choose a dilating instrument to suit the site of the stricture. Use generous amounts of lubricating gel. 2. For distal or meatal strictures, use short female dilating instruments, for example Canny Ryall dilators. 3. For more proximal strictures, use curved Clutton dilators. With the patient in lithotomy, hold the penis vertically. Introduce the dilator, point the penis towards the patient’s head and slowly advance the dilator. Push the curve of the dilator against the bulbar urethra and lower your hands. As you do this, the dilator will slide into the bladder. To confirm that you are in the bladder, rotate the dilator; if it rotates easily then you are in the right place.
Lower urinary tract
SUPRAPUBIC CATHETER INSERTION
Appraise
Anatomical considerations
Action
CYSTOSCOPY
Appraise
Action
OPERATIONS FOR URETHRAL STRICTURES
Appraise
URETHRAL DILATATION
Action
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Lower urinary tract