The ilioinguinal nerve is the collateral branch of the iliohypogastric, both being derived from the first lumbar nerve. It has no lateral but only a terminal cutaneous distribution. In the anterior abdominal wall it lies in the neurovascular plane between the internal oblique and transversus abdominis muscles and supplies their lower fibres. It then pierces internal oblique and passes down deep to the external oblique (see Fig. 5.7, p. 226) to emerge on the front of the cord through the superficial inguinal ring. Piercing the external spermatic fascia its chief distribution is to the skin of the root of the penis and the anterior one-third of the scrotum, but it supplies also a small area of thigh below the medial end of the inguinal ligament.
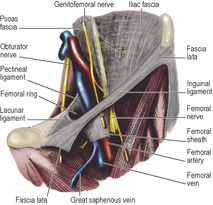
The genitofemoral nerve is derived from the first and second lumbar nerves, but fibres from only L1 pass into the femoral branch. This branch is given off from the nerve as it lies on psoas major. It runs down on the external iliac artery and passes beneath the inguinal ligament into the femoral sheath. It pierces the anterior wall of the sheath and the overlying fascia lata below the middle of the inguinal ligament (Fig. 3.1) to supply skin over the femoral triangle. The genital branch passes through the deep ring with the other constituents of the spermatic cord (see p. 228).
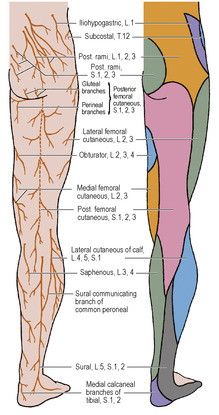
The medial femoral cutaneous nerve is a branch of the femoral nerve (L2, 3). Inclining medially across the femoral vessels it pierces the fascia lata at the mid-thigh and supplies the medial side of the thigh; its terminal twigs join the patellar plexus (see below).
The intermediate femoral cutaneous nerve (L2, 3) is also a branch of the femoral nerve. It passes vertically downwards, usually pierces sartorius, and then pierces the fascia lata at a higher level than the medial cutaneous nerve to supply the front of the thigh as far down as the knee, where its terminal twigs join the patellar plexus.
The lateral femoral cutaneous nerve is a branch of the lumbar plexus (L2, 3). Passing from the lateral border of psoas major across the iliac fossa it lies at first behind the fascia iliaca; but approaching the inguinal ligament it inclines forwards and is incorporated within the substance of the iliac fascia, which is here a thick tough membrane (Fig. 3.1). The nerve now passes behind or pierces the inguinal ligament a centimetre to the medial side of the anterior superior iliac spine (Fig. 3.2).
The nerve enters the thigh deep to the fascia lata, and divides into anterior and posterior branches which pierce the fascia lata separately. The anterior branch is distributed along the anterolateral surface of the thigh, and its terminal twigs enter the patellar plexus. The posterior branch supplies the skin on the posterolateral aspect from the level of the greater trochanter to the mid-thigh.
The nerve is sometimes compressed as it passes through the inguinal ligament, causing pain and altered sensation in the lateral side of the thigh (meralgia paraesthetica). Less commonly the nerve may be compressed as it passes through the iliac fascia. Surgical treatment of this condition requires division of the inguinal ligament and freeing the nerve of any fascial compression.
The obturator nerve (L2–4) sends a twig from its anterior division into the subsartorial plexus, whence cutaneous branches pass to skin over the medial side of the thigh (Figs 3.46 and 3.47).
Patellar plexus
This is a fine network of communicating twigs in the subcutaneous tissue over and around the patella and patellar ligament. It is formed by the terminal branches of the medial and intermediate femoral cutaneous nerves, anterior branch of the lateral femoral cutaneous nerve and infrapatellar branch of the saphenous nerve.
Superficial arteries
Four cutaneous branches of the femoral artery are found in the subcutaneous tissue below the inguinal ligament.
The superficial circumflex iliac artery pierces the fascia lata lateral to the saphenous opening and passes up below the inguinal ligament to the anastomosis at the anterior superior iliac spine.
The superficial epigastric artery emerges through the saphenous opening. It crosses the inguinal ligament and runs towards the umbilicus.
The superficial external pudendal artery emerges from the saphenous opening and passes medially, in front of the spermatic cord (round ligament) to the penis and scrotum (labium majus).
The deep external pudendal artery pierces the fascia lata and passes behind the spermatic cord (round ligament) to supply the skin of the scrotum (labium majus).
Superficial veins
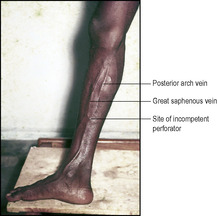
These are essentially tributaries of the great (long) saphenous vein, one of the most important veins in the body in view of its tendency to become dilated (varicose), and its use as a conduit in vascular surgery.
The great (long) saphenous vein, the longest vein in the body, begins as the upward continuation of the medial marginal vein of the foot (p. 145). It courses upwards in front of the medial malleolus (Fig. 3.31), crosses the lower quarter of the medial surface of the tibia obliquely and runs up behind the medial border of the tibia towards the knee, where it lies a hand’s breadth behind the medial border of the patella. It spirals forwards round the medial convexity of the thigh and ends by passing through the cribriform fascia covering the saphenous opening (Fig. 3.3), which lies about 3cm below and lateral to the pubic tubercle. Here it joins the femoral vein. It contains up to 20 valves, more of them below knee level than above. Incompetence of valves is a cause of varicosity of the vein.
A number of tributaries may be expected to join the great saphenous vein in the region of the saphenous opening; like venous patterns elsewhere the exact number is variable since some may unite with others to form common trunks or may be missing. There are usually four veins that correspond to the four cutaneous branches of the femoral artery (superficial circumflex iliac, superficial epigastric, and superficial and deep external pudendal). The superficial external pudendal artery runs horizontally between the superficial and deep external pudendal veins. The deep external pudendal artery runs medially behind the saphenous vein near its termination. Anterolateral and posteromedial veins of the thigh frequently join the great saphenous vein a little below the saphenous opening.
The superficial epigastric vein may form the lower end of the thoracoepigastric vein which serves as a communication between the superior and inferior venae cavae (see p. 179).
The deep connections of the lower end of the great saphenous vein in the leg are described on page 141.
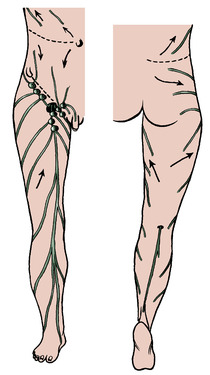
Lymph nodes and vessels
Large lymphatic vessels accompany the great saphenous vein from the foot, leg and thigh, and numerous large vessels spiral around the outer side of the thigh to converge on the superficial inguinal nodes (Fig. 3.4). These consist of about 10 nodes. A proximal group lies just distal to the inguinal ligament and a distal group lies vertically along the terminal great saphenous vein. The lateral nodes of the proximal group receive lymph from the buttock, flank and back below the waist. The medial nodes of this group receive lymph from the umbilicus and anterior abdominal wall below it, the external genitalia of both sexes (excluding the testis, but including the lower vagina), the lower anal canal and perineum, and a small proportion of the drainage from the uterus via lymphatics accompanying the round ligament. The distal group receives all the superficial lymphatics of the lower limb, except for those from the posterolateral part of the calf. The superficial inguinal nodes drain mainly to the external iliac nodes by efferent lymphatics, some of which pierce the cribriform fascia.
Three of four deep inguinal nodes lie deep to the fascia lata, medial to the femoral vein, one or two being in the femoral canal. They receive the deep lymphatics that accompany the femoral vessels from the popliteal fossa, lymphatics from the glans penis (or clitoris) and a few efferent lymphatics from the superficial inguinal nodes. The deep inguinal nodes drain to the external iliac nodes through the femoral canal.
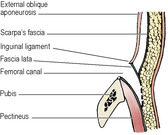
Superficial fascia
The membranous layer of the superficial fascia of the abdominal wall (see Scarpa’s fascia, p. 179) extends into the thigh and fuses with the fascia lata (Fig. 3.5) at the flexure skin crease of the hip joint (Fig. 4.1A, B, p. 180). The attachment extends laterally from the pubic tubercle below the inguinal ligament. The saphenous opening lies below this line, so a femoral hernia, emerging from the saphenous opening, can never come to lie in the space deep to Scarpa’s fascia. The hernia emerges into ordinary subcutaneous fat and therefore does not become very large.
Fascia lata
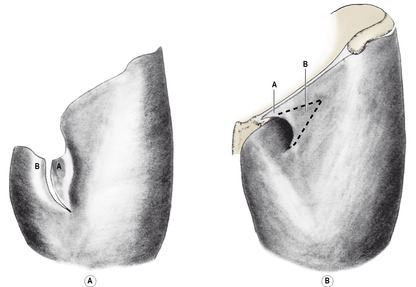
The deep fascia, the fascia lata, encloses the thighs like a stocking but one whose top is too large. A vertical slit has been cut at the top of the stocking, so to speak, and the cut edges overlapped to fit the bony pelvis, so forming the margin of the saphenous opening, as described below.
The upper end of the lateral part of the cut fascial stocking (Fig. 3.6A) is attached to the inguinal ligament, which it draws into a downward convexity when the thigh is extended. The line of fascial attachment extends posteriorly from the anterior superior iliac spine along the external lip of the iliac crest, splitting to enclose the tensor fasciae latae and gluteus maximus muscles. The two layers that enclose the gluteus maximus are very thin. Posterior to gluteus maximus the fascia lata is attached to the sacrum and the sacrotuberous ligament. The attachment of the fascia lata extends along the convexity of the ischial tuberosity and the ischiopubic ramus around the medial side of the limb to the body of the pubic bone.
The medial part of the cut fascial stocking (Fig. 3.6B) passes deep to the lateral part (A) over pectineus, posterior to the femoral sheath, and is attached to the pectineal line of the pubic bone. To change the simile, the edges of A and B of the slit in Figure 3.6 are overlapped like lapels of a double-breasted jacket and the great saphenous vein passes through the gap like a hand reaching into the inside pocket. The cut edge of A forms a crescentic or falciform margin to the saphenous opening, which is merely the oblique space lying between the cut edges as they overlap each other. The saphenous opening is covered in by a loose fascia attached laterally to the falciform edge and medially to the fascia lata where it lies over adductor longus. This fascia is pierced by the great saphenous vein and its tributaries and by efferent lymphatics from the superficial inguinal lymph nodes, giving it a sieve-like appearance, whence it derives the name of cribriform fascia.
The fascia lata is attached below to the tibial condyles and to the head of the fibula. Anteriorly it is reinforced by expansions from sartorius and quadriceps femoris. Over the popliteal fossa it is strengthened by transverse fibres and continues below into the deep fascia of the calf.
Tensor fasciae latae
This arises from a 5-cm length of the external lip of the iliac crest between the anterior superior iliac spine and the tubercle of the crest. It is a thin sheet of muscle at its origin and becomes thicker at its insertion into the iliotibial tract.
Nerve supply. By the superior gluteal nerve (L4, 5, S1).
Action. Its action is to pull upon the iliotibial tract, so assisting gluteus maximus in extending the knee joint. The muscle is also active in helping to stabilize the pelvis during walking, when it assists gluteus medius and minimus in resisting adduction at the hip (see p. 125).
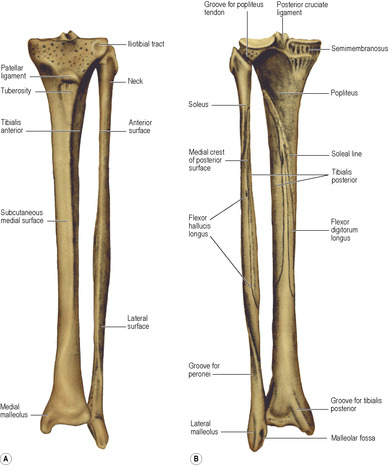
Iliotibial tract
This is a thickening of the fascia lata on the lateral side of the thigh. The upper end of the tract splits to enclose tensor fasciae latae and the superficial layer is attached to the iliac crest. Three-quarters of gluteus maximus is inserted into it. The tract passes vertically down and is inserted into Gerdy’s tubercle, a smooth circular facet on the lateral condyle of the tibia (Fig. 3.51A). When the knee is straight the tract passes in front of the axis of flexion. Thus it maintains the knee in the hyperextended position while the quadriceps is relaxed and the patella freely mobile.
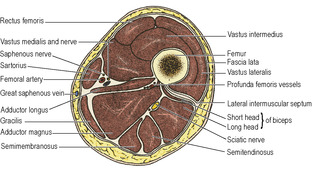
The lateral intermuscular septum is a strong layer extending from the deep surface of the iliotibial tract to the linea aspera of the femur. Vastus lateralis lies in front and the short head of biceps femoris behind it (Fig. 3.7).
Femoral triangle
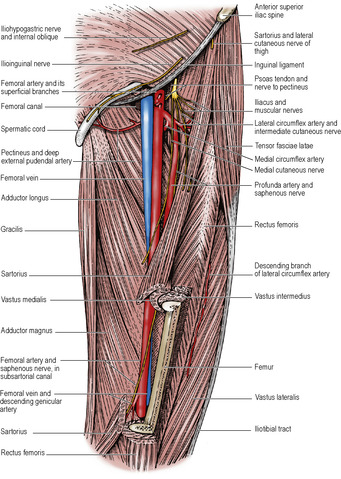
When the fascia lata is removed from the front of the thigh the underlying muscles are exposed (Fig. 3.2). The most superficial of all is sartorius, a parallel-sided ribbon of muscle that swings obliquely across the thigh. The adductor longus is prominent on the medial side, and the two muscles enclose, with the inguinal ligament, the femoral triangle.
The femoral triangle is defined as the triangle that lies between the inguinal ligament, the medial border of sartorius, and the medial border of adductor longus. The floor of the triangle is gutter-shaped and the hollow can be seen when the thigh is flexed. The femoral nerve and vessels lie in the gutter. The muscles lying in the floor of the femoral triangle are the iliacus, psoas, pectineus and adductor longus.
Sartorius
This muscle, the longest in the body, arises from the anterior superior iliac spine and the notch below it. Its parallel fibres extend for the whole length of the muscle. It crosses the thigh obliquely along the medial border of the femoral triangle (Fig. 3.2) and on the fascial roof of the adductor canal, and then descends more vertically to the upper part of the medial surface of the tibia. It is inserted here in front of gracilis and semitendinosus by an aponeurosis, the upper end of which arches backwards over the top of the gracilis and semitendinosus tendons.
Nerve supply. By a branch from the anterior division of the femoral nerve (L2–4).
Action. Sartorius draws the lower limb into the sitting tailor’s position (thigh flexed, laterally rotated and abducted, knee flexed).
Adductor longus is described with the other adductors on page 121.
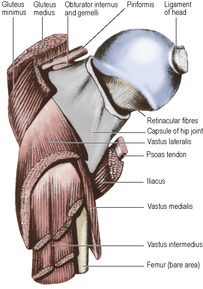
Iliacus
This muscle arises from the iliac fossa (see p. 274). Entering the thigh beneath the lateral part of the inguinal ligament, it curves backwards behind the femoral vessels to be inserted into the front of the psoas tendon (Fig. 3.8) and a small area of femoral shaft just below the lesser trochanter. The lower part of the iliac fossa is occupied by a bursa, the iliac (psoas) bursa, which lies deep to iliacus and psoas and extends with them into the upper thigh.
Nerve supply. By the femoral nerve (L2, 3) in the iliac fossa.
Action. With psoas, it is a powerful flexor of the hip joint (see p. 129).
Psoas major
This arises from the lumbar spine (see p. 272). It passes into the thigh deep to the middle of the inguinal ligament. Its rounded tendon is inserted into the lesser trochanter (Fig. 3.8). Both iliacus and psoas pass across the front of the capsule of the hip joint, with the bursa intervening. The bursa may communicate with the hip joint through a gap in the capsule that lies between the iliofemoral and pubofemoral ligaments.
Nerve supply. By the anterior rami of the first three lumbar nerves (mainly L2).
Action. With iliacus it is a powerful flexor of the hip. The action of psoas on the lumbar spine is described on page 272.
Pectineus
This is a quadrilateral muscle that arises from the pectineal line of the pubis and from a narrow area of bone below (Fig. 3.11). It slopes backwards down to the upper end of the femoral shaft, where it is inserted into a vertical line behind and below the lesser trochanter (Fig. 3.12). The muscle is covered anteriorly by an infolding of fascia lata that passes deep to the falciform margin of the saphenous opening (Fig. 3.6B). The femoral vein and femoral canal lie on the surface of the muscle, while adductor brevis and the anterior division of the obturator nerve lie behind it.
 |
| Figure 3.11 |
Nerve supply. By the anterior division of the femoral nerve (L2, 3) by a branch that passes behind the femoral sheath. Occasionally it receives a twig from the anterior division of the obturator nerve (L2, 3).
Action. Pectineus flexes and adducts the thigh.
Femoral sheath
The femoral vessels, passing beneath the inguinal ligament, draw around themselves a funnel-shaped prolongation of the transversalis fascia in front and the psoas fascia behind (Fig. 3.1). This prolongation of fascia, the femoral sheath, fuses with the adventitia of the artery and vein about 3cm distal to the inguinal ligament.
The femoral nerve in the iliac fossa lies in the gutter between psoas and iliacus, behind the iliac fascia. Lateral to the femoral sheath the transversalis fascia and iliac fascia fuse with the inguinal ligament, and the femoral nerve thus enters the thigh outside the femoral sheath. Within the sheath the femoral artery is lateral to the femoral vein and there is a space on the medial side of the vein, the femoral canal (Fig. 3.2). The femoral canal is widest at its abdominal end, where its opening, the femoral ring, has four boundaries. Anteriorly lies the medial part of the inguinal ligament, medially the crescentic edge of the lacunar ligament, posteriorly the pectineal ligament and laterally the femoral vein (Fig. 3.1). A femoral hernia enters the femoral canal through this ring. The lacunar ligament may have to be incised to release a strangulated hernia, and here an accessory (abnormal) obturator artery is at risk (see p. 309). The canal contains a lymph node (of Cloquet) which in the female drains directly from the clitoris, and in the male from the glans penis.
Femoral artery
The artery enters the thigh at a point midway between the anterior superior iliac spine and the pubic symphysis (midinguinal point). Here it lies on the psoas major tendon, which separates the artery from the capsule of the hip joint. This is the position where its pulsation can be felt and where it can be entered for arterial catheterization. It emerges from the femoral sheath, courses downwards and enters the adductor canal deep to sartorius. It has four small branches below the inguinal ligament (see p. 112) and just below the termination of the femoral sheath gives off a large branch, the profunda femoris, the chief artery of the thigh.
The surface marking of the femoral artery, with the hip slightly flexed and laterally rotated, is from the midpoint between the pubic symphysis and the anterior superior iliac spine, along the upper two-thirds of a line towards the adductor tubercle. The surgical approach to the artery in the adductor canal is through an incision on the medial aspect of the lower thigh; sartorius is retracted medially and the fascial roof of the canal divided.
Cannulation. The femoral artery is second only to the radial (see p. 69) as the site of choice for the placement of an arterial line. Its superficial position below the inguinal ligament makes it easily accessible. The most common complications include retroperitoneal haemorrhage and perforation of the gut (by entering the abdominal cavity), and arteriovenous fistula (with the femoral or external iliac vein).
The profunda femoris artery is normally the vessel of supply for all thigh muscles (unless its circumflex branches come directly from the femoral). It usually arises from the lateral side of the femoral artery about 3–4cm distal to the inguinal ligament and then spirals down deep to it, passing between pectineus and adductor longus, whose upper border separates the femoral and profunda arteries (Fig. 3.2). The profunda vein lies in front of the profunda artery and turns medially to pass through the angle between the femoral artery and its profunda branch to drain into the femoral vein. The profunda artery continues down on adductor brevis and magnus and ends as the fourth perforating artery. Apart from the perforating arteries and muscular branches, it gives off large lateral and medial circumflex femoral arteries.
The lateral circumflex femoral artery arises from the lateral side of the profunda artery (Fig. 3.2) or occasionally from the femoral artery. It passes laterally between the branches of the femoral nerve, and disappears from the femoral triangle beneath sartorius to lie deep to rectus femoris. Here it breaks up into three branches.
The ascending branch runs up on the vastus lateralis, under cover of sartorius and tensor fasciae latae. It gives a branch to the trochanteric anastomosis (see p. 126) and passes on towards the anterior superior iliac spine, where it ends by anastomosing with the superficial and deep circumflex iliac, an iliac branch of the iliolumbar and the superior branch of the superior gluteal artery. This ascending branch is a large vessel and in the anterior approach to the hip joint between sartorius and tensor fasciae latae, it and its venae comitantes must be secured when separating the muscles.
The transverse branch passes across the vastus lateralis and winds around the femur to form one limb of the cruciate anastomosis (see p. 126).
The descending branch slopes steeply downwards, with the nerve to vastus lateralis, in a groove between the anterior edge of the vastus lateralis and the vastus intermedius. It supplies both muscles and ends by sending twigs to the anastomosis around the knee.
The medial circumflex femoral artery arises from the medial side of the profunda (occasionally from the femoral), often above its lateral companion, and immediately passes backwards between pectineus and the psoas tendon. Running above adductor brevis and below obturator externus, it passes between quadratus femoris and adductor magnus to enter the gluteal region. It gives an ascending branch to the trochanteric anastomosis, and a horizontal branch to the cruciate anastomosis.
The four perforating arteries pass backwards through adductor magnus, the first having passed above, the second through and the third and fourth below adductor brevis. They supply the adductor muscles and the hamstrings and make a series of anastomoses with one another, with the cruciate anastomosis above and with the popliteal artery below.
In the vascular surgical literature, the femoral artery above the origin of the profunda branch (deep femoral artery) is termed the common femoral artery, and the vessel below this branch is the superficial femoral artery.
Femoral vein
The vein enters the lower angle of the femoral triangle, where it lies posterior to the artery. It ascends through the femoral triangle and comes to lie on the medial side of the artery. It receives the profunda femoris vein posteriorly and just below the femoral sheath the great saphenous vein joins it anteriorly (Fig. 3.1). Within the sheath it passes under the inguinal ligament and runs along the brim of the pelvis as the external iliac vein. It has four or five valves, the most constant ones being just above the junctions with the profunda and great saphenous veins. Absence of these valves could contribute to the development of varicosity of the great saphenous vein.
In the living body the position of the femoral vein below the inguinal ligament is found by feeling the pulsations of the femoral artery, which is immediately lateral to the vein. In thin people the femoral vein may be surprisingly near the surface even though it is within the femoral sheath.
Femoral nerve
This is the nerve of the extensor compartment of the thigh, and is formed from the posterior divisions of the anterior rami of the lumbar nerves 2, 3 and 4. The obturator nerve, which supplies the adductor muscles derived from the flexor muscles of the thigh, is formed by the anterior divisions of the same rami (see p. 13). The femoral nerve supplies iliacus in the abdomen. Lying in the iliac fossa between psoas and iliacus the femoral nerve enters the thigh by passing deep to the inguinal ligament at the lateral edge of the femoral sheath, which separates it from the femoral artery (Fig. 3.1).
As it enters the femoral triangle it gives a branch to pectineus; this branch passes behind the femoral sheath to reach the muscle (Fig. 3.2). Just distal to the inguinal ligament the femoral nerve divides into several branches. The intermediate and medial femoral cutaneous nerves have already been described (see p. 112).
There are two nerves to sartorius, one of which usually pierces the muscle and continues as the intermediate cutaneous nerve. The nerve to rectus femoris is usually double; the upper nerve gives a branch to the hip joint. The nerve to vastus medialis, the largest of the muscular branches, passes down on the lateral side of the femoral artery into the adductor canal, where it gives branches to and enters vastus medialis, and continues downwards to the capsule of the knee joint. The nerve to vastus lateralis runs downwards with the descending branch of the lateral femoral circumflex artery to supply the muscle and the knee joint. The nerve to vastus intermedius enters the anterior surface of the muscle and also supplies the knee joint. The saphenous nerve leaves the femoral triangle at its lower angle and in the subsartorial canal passes across the front of the femoral artery to reach its medial side (Fig. 3.2). It gives twigs to the subsartorial plexus and leaves the canal at its distal end by passing between sartorius and gracilis.
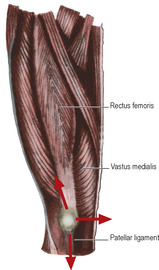
Quadriceps femoris
This muscle is the main extensor of the knee joint and has four parts—rectus femoris and the three vastus muscles: lateralis, intermedius and medialis. All converge to form the quadriceps tendon which contains the patella and which continues down as the patellar ligament (tendon) to be inserted into the tuberosity of the tibia.
Rectus femoris arises from the ilium by two heads (Fig. 3.48). The reflected head arises from a groove above the acetabulum, the straight head from the upper half of the anterior inferior spine, above the iliofemoral ligament. The two heads unite to form the anterior lamina of the quadriceps tendon. The posterior surface of the muscle is clad in a glistening aponeurosis that glides on the anterior surface of vastus intermedius. The anterior surface is covered with a similar aponeurosis on its upper part.
 |
| Figure 3.48 |
Vastus lateralis has an extensive linear origin from the upper part of the intertrochanteric line, the greater trochanter (Fig. 3.8) and the lateral lip of the linea aspera of the femur. It also arises from the lateral intermuscular septum. Inferiorly the muscle is incorporated in the quadriceps tendon (Fig. 3.10). The anterior edge of the muscle lies free on vastus intermedius; the descending branch of the lateral circumflex artery and the nerve to vastus lateralis lie in the shallow gutter between the two.
Vastus intermedius arises from the anterior and lateral surfaces of the upper two-thirds of the shaft of the femur. The anterior surface of the muscle is covered by an aponeurosis which is continued down into the quadriceps tendon.
Articularis genu is a small muscle which arises from the anterior surface of the lower femoral shaft, deep to vastus intermedius, and is inserted into the upper convexity of the suprapatellar bursa (see p. 139).
Vastus medialis arises from the lower part of the intertrochanteric line and the medial lip of the linea aspera and from the tendon of adductor magnus below the hiatus for the femoral vessels. The muscle slopes around the medial surface of the femur, merging with vastus intermedius, and is continuous below with the quadriceps tendon, while the lowest fibres, lying nearly horizontal, are inserted directly into the medial border of the patella. These fibres are indispensable to the stability of the patella (Fig. 3.10).
The quadriceps tendon is attached to the base and sides of the patella. A thin sheet passes across the front of the patella into the patellar ligament and the retinacula.
The patellar ligament (tendon) connects the lower border of the patella with the smooth convexity on the tuberosity of the tibia (Fig. 3.51). It represents the continuation of the quadriceps tendon. The patellar retinacula are fibrous expansions from the quadriceps tendon and patellar ligament, which connect the sides of the patella with the condyles of the tibia and the collateral ligaments. The lateral retinaculum is reinforced by the iliotibial tract.
Nerve supplies. Each muscle is supplied by its own branch from the femoral nerve (L3, 4).
Actions. The muscle is the main extensor of the knee joint. Rectus femoris can assist iliopsoas to flex the hip.
Test. While lying on the back with the knee partly flexed, the patient extends the knee against resistance. Rectus femoris can be seen and felt contracting.
Stability of the patella
The patella is a sesamoid bone in the quadriceps tendon. It is mobile from side to side. The patellar ligament is vertical, but the pull of the quadriceps is oblique, in the line of the shaft of the femur, and when the muscle contracts it tends to draw the patella laterally. Three factors discourage this lateral dislocation; they are the usual bony, ligamentous and muscular factors that control the stability of any bone. The bony factor consists in the forward prominence of the lateral condyle of the femur (Fig. 3.9), the ligamentous factor is the tension of the medial patellar retinaculum, but they are in themselves incapable of preventing lateral displacement of the patella. The lowest fibres of vastus medialis, inserted into the border of the bone, hold the patella medially when the quadriceps contracts (Fig. 3.10). These fibres of vastus medialis are indispensable to the stability of the patella.
Adductor canal
This canal (also known as the subsartorial or Hunter’s canal) is a gutter-shaped groove between vastus medialis and the front of the adductor muscles, below the apex of the femoral triangle. The gutter is roofed in by a fascia which contains in its meshes the subsartorial plexus. The canal so formed contains the femoral artery and vein, the saphenous nerve and, in the upper part, the nerve to vastus medialis (Fig. 3.7). Sartorius lies on the fascial roof. The adductors in the floor of the canal are the adductor longus above and the adductor magnus below. The subsartorial plexus receives small branches from the medial cutaneous nerve of the thigh, the saphenous nerve and the anterior division of the obturator nerve. The plexus supplies the overlying fascia lata and an area of skin above the medial side of the knee. The femoral artery leaves the canal by passing into the popliteal fossa through the hiatus between the hamstring and adductor parts of the adductor magnus muscle. In the distal part of the canal the femoral vein is posterolateral to the artery. The vein ascends posteriorly until in the femoral triangle it lies medial to the artery. This is in keeping with the rotation medially of the lower limb from the fetal position, and is further reflected in the spiral manner in which the saphenous nerve passes across the femoral artery. At all levels in the thigh the artery lies between saphenous nerve and femoral vein. Below the opening in the adductor magnus the saphenous nerve continues to descend in the canal. The descending genicular artery arises from the femoral artery just above the adductor hiatus and, passing downwards, divides into a superficial saphenous artery that accompanies the saphenous nerve and a deep muscular branch that enters the vastus medialis and joins the arterial anastomosis around the knee.
The saphenous nerve passes out of the canal by escaping from behind the posterior border of sartorius (in front of gracilis). It pierces the fascia lata here and passes downwards behind the great saphenous vein (Fig. 3.3). Just before leaving the canal the infrapatellar branch is given off; this nerve pierces sartorius, joins the patellar plexus and supplies prepatellar and infrapatellar skin.
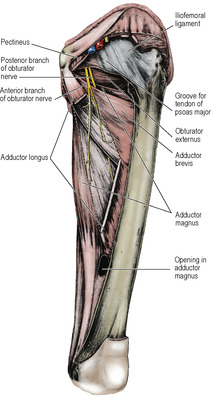
Part two. Medial compartment of the thigh
The contents of this (adductor) compartment of the thigh are separated from the anterior (extensor) compartment by the medial intermuscular septum, but there is no septum dividing them from the posterior (flexor or hamstring) compartment. The muscles consist of gracilis and the three adductors, longus, brevis and magnus, while deeply lies obturator externus. The nerve of the compartment is the obturator, and the artery is the profunda femoris, assisted proximally by the obturator artery.
The medial intermuscular septum is a thin fascia that lies between vastus medialis and the adductors and pectineus. It is attached to the fascia lata and the linea aspera of the femur, and is continuous above with the fascia on pectineus (see p. 115).
Gracilis
This, the most superficial muscle of the medial side of the thigh (Fig. 3.2), arises as a flat sheet from the edge of the inferior ramus of the pubis and the adjoining ischial ramus (Fig. 3.48). The muscle narrows in triangular fashion and is replaced by a cylindrical tendon which is inserted into the upper part of the medial surface of the shaft of the tibia just behind sartorius. The gracilis receives a segmental blood supply from the medial circumflex, profunda and femoral arteries in succession distally. A gracilis muscular flap based on the profunda pedicle is used in perineal reconstructive surgery.
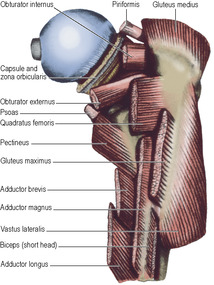
Adductor longus
This, the most superficial of the three adductors, arises from a circular area on the body of the pubis, in the angle between the pubic crest and symphysis (Fig. 3.48), by a strong round tendon, sometimes ossified (‘rider’s bone’). The muscle rapidly becomes fleshy and flattens out to be inserted by an aponeurotic flat tendon into the middle third of the linea aspera of the femur (Fig. 3.11).
Adductor brevis
This muscle arises from the body and inferior ramus of the pubic bone, deep to pectineus and adductor longus (Fig. 3.48). It widens in triangular fashion to be inserted into the upper part of the linea aspera immediately behind the insertion of pectineus and adductor longus. The anterior division of the obturator nerve passes vertically downwards on its anterior surface (Fig. 3.11); the posterior division passes down behind it. The upper border of adductor brevis thus lies between the two divisions of the obturator nerve in the same way as the upper border of adductor longus lies between the femoral and the profunda femoris vessels.
Adductor magnus
This is a composite muscle formed by the fusion of adductor and hamstring muscle masses, each with their own nerve supply.
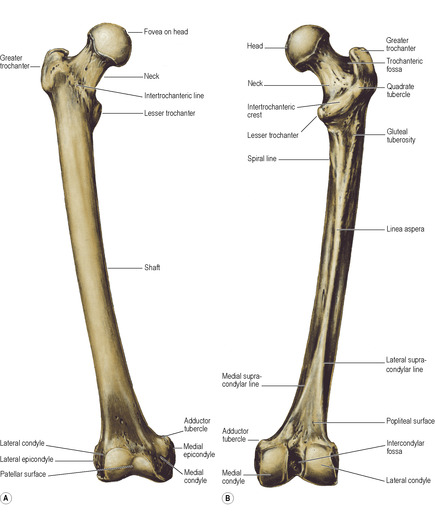
The hamstring part arises from the ischial tuberosity (Fig. 3.48), and the fibres pass vertically downwards to a tendinous attachment to the adductor tubercle of the femur, with an expansion to the medial supracondylar line. In continuity with the ischial origin, the adductor part arises from the ischiopubic ramus. These fibres are inserted progressively higher along the medial supracondylar line, the linea aspera and up to the gluteal tuberosity (Fig. 3.50B). The upper border of the muscle is horizontal, lying edge to edge with the lower border of quadratus femoris, and the medial circumflex femoral artery passes between the two muscles from front to back to reach the cruciate anastomosis (Fig. 3.13). Near the top of the medial supracondylar line there is a gap in the muscle attachment through which the femoral vessels pass, changing their name to popliteal as they do so. Along the linea aspera attachment there are four small openings, the lowest for the end of the profunda femoris vessels, and the others for their perforating branches.
Nerve supplies of adductors. Gracilis and adductor longus and brevis are supplied by the anterior division of the obturator nerve, the hamstring part of magnus by the tibial part of the sciatic nerve and the rest of magnus by the posterior division of the obturator (L2, 3 for all muscles).
Actions of adductors. The adductor mass of muscles, though large, is less important in the prime movement of adduction than in synergic activities associated with posture and gait.
Tests for adductors. While lying on the back with the knee straight, the patient adducts the thigh against resistance, and the upper ends of gracilis and adductor longus are palpated.
Obturator externus
This muscle arises from the whole of the obturator membrane and from the anterior bony margin of the obturator foramen. Both membrane and muscle fall short of the obturator notch above, thereby forming a canal for the passage of the obturator nerve and vessels (Fig. 3.11). The muscle passes laterally and posteriorly beneath the neck of the femur where it narrows into a tendon that spirals in contact with the back of the femoral neck to be inserted on the medial surface of the greater trochanter into a deep pit, the trochanteric fossa. The capsule of the hip joint encloses the back of the neck of the femur only as far as the place where obturator externus tendon is in contact with periosteum, namely half the neck of the femur (Fig. 3.12), whereas in front the capsule of the hip joint includes the whole of the neck of the femur (Fig. 3.8).
Nerve supply. By the posterior division of the obturator nerve (L3, 4).
Action. With the other short muscles around the hip joint, it stabilizes and supports the proximal part of the limb. As its line of pull passes behind the hip joint, it is a lateral rotator of the femur.
Obturator artery and nerve
The obturator artery, on emerging from the obturator foramen with the nerve, divides into anterior and posterior branches that encircle the foramen between the obturator externus and the membrane. They anastomose with each other and with the medial circumflex artery. From the posterior branch the articular twig to the hip joint arises; it enters the acetabular notch and runs in the ligament of the head of the femur to supply a small scale of bone in the region of the pit for the attachment of the ligament (see p. 129).
The obturator nerve divides in the obturator notch into anterior and posterior divisions; the anterior passes above obturator externus, the posterior passes through the muscle, giving off a branch to supply it before doing so.
The anterior division, giving an articular branch to the hip joint, descends in the thigh behind the adductor longus, which it supplies. Passing over the anterior surface of adductor brevis (Fig. 3.11), which it usually supplies, it goes on to supply gracilis and end in the subsartorial plexus, whence branches supply the skin over the medial side of the thigh. Direct branches to the skin are often given off at a level above the subsartorial plexus.
The posterior division emerges through obturator externus (having already supplied that muscle), and passes vertically downwards on adductor magnus deep to the other adductor muscles. It supplies adductor magnus and gives a terminal branch which runs with the femoral artery through the hiatus in the muscle to the popliteal fossa and supplies the capsule of the knee joint by passing in with the middle genicular artery. The posterior division may supply adductor brevis when this is not supplied by the anterior division.
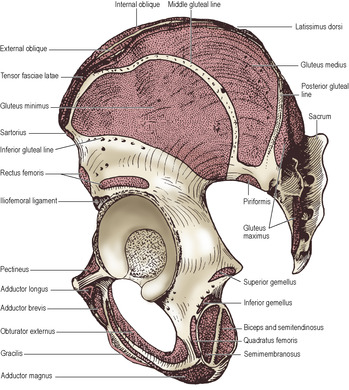
Part three. Gluteal region and hip joint
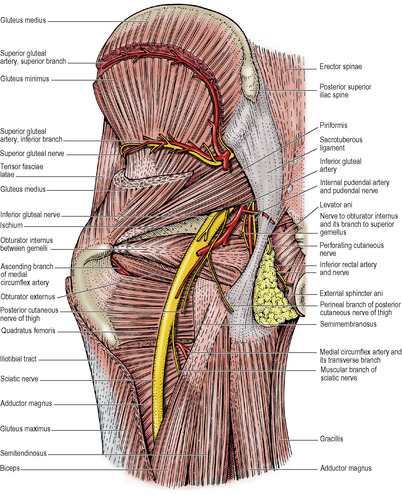
The gluteal region or buttock lies behind the pelvis, and extends from the iliac crest to the gluteal fold (fold of the buttock). Various muscles, nerves and vessels emerge from the pelvis to enter the lower limb in this region. The muscles of the region are the three gluteal—gluteus maximus, medius and minimus—and the deeply placed piriformis, obturator internus, superior and inferior gemellus, and quadratus femoris (Fig. 3.13). Bony and ligamentous features of the region include the back of the sacrum and hip bone, the upper end of the femur, and the sacrotuberous and sacrospinous ligaments. The greater sciatic foramen is formed above and in front by the greater sciatic notch of the hip bone, behind by the sacrotuberous ligament, and below by the sacrospinous ligament (see Figs 5.73 and 5.74, pp. 323 and 324). The lesser sciatic foramen is formed by the lesser sciatic notch of the hip bone, and the same two ligaments. The ligaments cross each other and so convert the two sciatic notches into foramina.
Subcutaneous tissue
The subcutaneous fat is well developed in the gluteal region and gives the buttock its characteristic convexity. The fold of the buttock is the transverse skin crease for the hip joint and is not caused by the lower border of the gluteus maximus, which crosses the line of the fold obliquely. The blood supply of the skin and fat is derived from branches of the superior and inferior gluteal arteries, and the lymphatic drainage is into the lateral group of the superficial inguinal lymph nodes.
The cutaneous nerves of the buttock (Fig. 3.47) are derived from posterior and anterior rami. The posterior rami of the upper three lumbar nerves slope downwards over the iliac crest to supply the upper skin of the buttock. The posterior rami of all five sacral nerves are cutaneous. The upper three supply the skin of the natal cleft, the lower two, with the coccygeal nerve, supply skin over the coccyx.
The anterior rami are derived from widely separated segments. The upper part of the lateral skin is supplied by lateral cutaneous branches of the subcostal and iliohypogastric nerves (T12 and L1), the lower part by branches of the lateral femoral cutaneous nerve (L2). The perforating cutaneous nerve (S2, 3) and branches of the posterior femoral cutaneous nerve (S2, 3) supply the lower central part of the buttock. Thus the segments between L2 and S2 are not represented in the skin of the buttock; their dermatomes lie peripherally, in the skin of the limb (see Fig. 1.9, p. 14). The posterior axial line lies between these discontinuous dermatomes.
Gluteus maximus
This is the largest and the most superficial of the gluteal muscles, and it is characterized by its large fibre bundles. A thick flat sheet of muscle, it slopes from the pelvis down across the buttock at 45° (see Fig. 2.4, p. 40). It arises from the gluteal surface of the ilium behind the posterior gluteal line, from the lumbar fascia, from the lateral mass of the sacrum below the auricular surface, and from the sacrotuberous ligament. The deep half of its lower half is inserted into the gluteal tuberosity of the femur (Fig. 3.12). The remaining three-quarters of the muscle is inserted into the upper end of the iliotibial tract (Fig. 3.13).
There are usually three bursae beneath the muscle: one over the ischial tuberosity, one over the greater trochanter, and another over vastus lateralis.
The blood supply comes from both the superior and inferior gluteal arteries, and the veins form a plexus beneath the muscle.
Nerve supply. By the inferior gluteal nerve (L5, S1, 2), the only muscle supplied by this nerve.
Action. Its action on the femur is a combination of lateral rotation and extension at the hip joint, while through the iliotibial tract its contraction supports the extended knee. In paralysis of quadriceps femoris it can become an active but weak extensor of the knee. It can be felt in contraction in standing with hip and knee each slightly flexed, in which case it is a powerful antigravity muscle. It comes into play as an extensor of the hip joint chiefly at the extremes of hip movement, as in running, climbing stairs, etc., and it is called into play little if at all in the mid-position of the hip joint, as in quiet walking, when the main extensors of the hip are the hamstrings. It is the chief antigravity muscle of the hip during the act of sitting down from standing, controlling flexion of the hip joint.
Test. While lying face down with the leg straight, if the patient tightens the buttock and extends the hip, the contracting muscle can be observed and palpated.
Gluteus medius
This muscle arises from the gluteal surface of the ilium between the middle and posterior gluteal lines (Fig. 3.48). Its posterior third is covered by the gluteus maximus (see Fig. 2.4, p. 40) and its anterior two-thirds by thick deep fascia. The muscle converges to a flat tendon which is attached to the lateral surface of the greater trochanter (Fig. 3.12). A bursa separates the tendon from the upper part of the lateral surface of the greater trochanter.
Gluteus minimus
This muscle arises under cover of gluteus medius (Fig. 3.13) from the gluteal surface of the ilium between the middle and inferior lines, whence its fibres converge to a tendon which is attached to the anterior surface of the greater trochanter (Fig. 3.8). Its anterior border lies edge to edge with that of gluteus medius from origin to insertion. A bursa separates the tendon from the medial part of the anterior surface of the greater trochanter.
Nerve supplies. Gluteus medius and minimus are supplied by the superior gluteal nerve (L4, 5, S1).
Actions. These two muscles abduct the hip joint and their anterior fibres rotate the thigh medially. The two muscles are constantly called into play as the foot on one side is raised during walking and running, when the muscles on the opposite (supporting) side contract to prevent the pelvis from sagging on the unsupported side. In this they are assisted by tensor fasciae latae (see p. 116). If they are paralysed the gait is markedly affected, the trunk swaying from side to side towards the weight-bearing limb to prevent downward tilting of the pelvis on the unsupported side.
Test. While lying face down with the leg flexed to a right angle, the patient turns the foot outwards against resistance. Gluteus medius is palpated below the iliac crest behind tensor fasciae latae, which can also be felt contracting. In the Trendelenburg test with the patient standing on one leg, the pelvis on the opposite side should rise slightly; if it falls due to loss of abductor power on the supporting side, the test is positive.
Piriformis
This is an important muscle in that its relations provide the key to the arrangement of the structures in the gluteal region (Fig. 3.13). The muscle arises from the front of the middle three pieces of the sacrum, within the pelvis, and passes laterally behind the sacral plexus to emerge through the greater sciatic foramen, which it almost completely fills. Some additional fibres arise from the upper margin of the notch (Fig. 3.48). In the buttock its upper border lies alongside gluteus medius, its lower border above the superior gemellus. It converges into a rounded tendon which is inserted into the medial surface of the upper border of the greater trochanter (Fig. 3.12).
The surface marking of the lower border of piriformis is from the midpoint of a line between the posterior superior iliac spine (indicated by an overlying dimple on the surface of the back) and the tip of the coccyx to the tip of the greater trochanter.
Nerve supply. By the anterior rami of S1 and S2.
Obturator internus and gemelli
Obturator internus arises from the internal surface of the lateral wall of the pelvis (see p. 289) and makes a right-angled bend around the lesser sciatic notch of the ischium to enter the gluteal region (Fig. 3.13). Its deep tendinous surface is separated by a bursa from the lesser sciatic notch, which is covered here by hyaline cartilage. As the muscle emerges into the buttock it is reinforced by additional muscle fibres arising from the margins of the lesser sciatic notch. These are the superior and inferior gemelli. They blend with the tendon of obturator internus, which is inserted into the medial surface of the greater trochanter above the trochanteric fossa (Fig. 3.12).
Nerve supply. By its own nerve (L5, S1, 2).
The superior gemellus arises from the spine of the ischium and is supplied by the nerve to obturator internus, while the inferior gemellus arises from the ischial tuberosity at the margin of the lesser sciatic notch and is supplied by the nerve to quadratus femoris (Fig. 3.48).
The tendon of obturator internus and the gemelli lie horizontal in the buttock, the superior gemellus below piriformis and the inferior gemellus above quadratus femoris. The sciatic nerve passes down on their posterior surface.
Quadratus femoris
This rectangular muscle (Fig. 3.13) arises from the ischial tuberosity and is inserted into the quadrate tubercle of the femur. It is separated from the back of the neck of the femur by the tendon of obturator externus. The upper and lower borders of this horizontal muscle lie edge to edge with the inferior gemellus above and the upper border of adductor magnus below.
Nerve supply. By its own nerve (L4, 5, S1).
Actions. Piriformis, obturator internus, the gemelli and quadratus femoris act together to adjust and stabilize the joint. Acting as prime movers they are lateral rotators of the extended thigh and abductors of the flexed thigh.
A number of structures emerge from the pelvis through the greater sciatic foramen into the gluteal region; to do so they pass above or below the piriformis muscle. Above the upper border emerge the superior gluteal nerve and vessels. Below the lower border emerge the inferior gluteal nerve and vessels, the pudendal nerve and vessels, the nerve to obturator internus, and the sciatic nerve with the posterior femoral cutaneous nerve on its surface and the nerve to quadratus femoris deep to it.
The superior gluteal nerve (L4, 5, S1) emerges from the greater sciatic notch above the upper border of piriformis and immediately disappears beneath the posterior border of gluteus medius and runs forwards between gluteus medius and minimus (Fig. 3.13). It supplies both muscles and ends in tensor fasciae latae. It has no cutaneous distribution.
The superior gluteal artery emerges from the pelvis above the upper border of piriformis and divides into superficial and deep branches. The superficial branch enters the deep surface of gluteus maximus to supply it and the overlying skin. The deep branch passes laterally between gluteus medius and minimus and divides into an upper and a lower branch. The upper reaches the anastomosis at the anterior superior iliac spine; the lower supplies the two glutei and joins the trochanteric anastomosis.
The inferior gluteal nerve (L5, S1, 2) leaves the pelvis beneath the lower border of piriformis and sinks into the deep surface of gluteus maximus (Fig. 3.13). It has no cutaneous distribution.
The inferior gluteal artery appears in the buttock between piriformis and the superior gemellus. It breaks up into muscular branches which supply piriformis, obturator internus, and gluteus maximus. It sends anastomotic branches to the trochanteric and cruciate anastomoses. One branch, the artery to the sciatic nerve, runs down on the sciatic nerve which it supplies. Cutaneous branches supply the buttock and back of thigh.
Trochanteric anastomosis
This provides the main source of blood for the supply of the head of the femur. The anastomosis lies near the trochanteric fossa (Fig. 3.50B). It is formed by anastomosis of the descending branch of the superior gluteal artery with the ascending branches of both lateral and medial circum-flex femoral arteries. The inferior gluteal artery usually joins the anastomosis. Branches from the anastomosis pass along the femoral neck with the retinacular fibres of the capsule (see p. 127).
Cruciate anastomosis
At the level of the middle of the lesser trochanter the transverse branch of the medial circumflex femoral artery meets the transverse branch of the lateral circumflex femoral at the lower border of the insertion of quadratus femoris. They are joined by an ascending branch of the first perforating artery and the cross is completed above by a descending branch of the inferior gluteal artery.
The pudendal nerve (S2–4) makes a brief appearance in the buttock (Fig. 3.13). On emerging from beneath piriformis the nerve turns forward around the back of the sacrospinous ligament, on which it lies just medial to the spine of the ischium. It leaves the buttock by passing forward through the space between the sacrotuberous and sacrospinous ligaments (the lesser sciatic foramen) to enter the pudendal canal (see Fig. 5.70, p. 316).
The internal pudendal artery follows a similar course to that of the nerve, lying on its lateral side. It crosses the tip of the ischial spine, against which it can be compressed to control arterial haemorrhage in the perineum. A companion vein lies on each side of the artery.
The nerve to obturator internus (L5, S1, 2) lies still more laterally and loops around the base of the ischial spine as it passes forward to sink into the muscle in the side wall of the ischioanal fossa (see Fig. 5.70, p. 316). It also supplies the superior gemellus.
The sciatic nerve (L4, 5, S1–3) emerges from below the piriformis muscle more laterally than the inferior gluteal and pudendal nerves and vessels (Fig. 3.13). It lies upon the ischium over the posterior part of the acetabulum. It is in contact with bone at a point one-third of the way up from the ischial tuberosity to the posterior superior iliac spine; this point is the surface marking for the entry of the nerve into the gluteal region. It passes vertically down over the posterior surface of obturator internus and quadratus femoris to the hamstring compartment of the thigh, where it is crossed posteriorly by the long head of biceps femoris. In the buttock it lies under cover of gluteus maximus just to the medial side of the midpoint between the greater trochanter and the ischial tuberosity, which is the surface marking of the nerve at the top of the thigh.
Its tibial and common peroneal (fibular) components usually separate in the upper part of the popliteal fossa but occasionally there is a high division and the two components may leave the pelvis separately, in which case the common peroneal nerve (L4, 5, S1, 2) usually pierces the piriformis while the tibial nerve (L4, 5, S1–3) emerges from beneath the muscle in the ordinary way.
The posterior femoral cutaneous nerve (S1–3) emerges from beneath piriformis and in its course in the buttock it lies on the sciatic nerve under cover of gluteus maximus. Below the buttock the nerve passes vertically down the midline of the back of the thigh and leg as low as the mid-calf. It lies beneath the fascia lata, superficial to the hamstrings, which separate it from the sciatic nerve, and supplies the fascia and overlying skin by a series of branches. Gluteal branches curl around the lower border of gluteus maximus to supply skin over the convexity of the buttock (Fig. 3.47). The long perineal branch winds medially and forward between gracilis and the fascia lata at the root of the limb to supply the posterior part of the scrotum or labium majus.
It is significant that the segments (S2, 3) of this nerve are also those of the pelvic parasympathetic nerves which supply pelvic viscera. Pain from pelvic disease may therefore be referred over the distribution of the posterior femoral cutaneous nerve, and such pain along the back of the thigh and upper calf must be distinguished from sciatica due to compression of the roots of the sciatic nerve.
The nerve to quadratus femoris (L4, 5, S1) lies on the ischium deep (anterior) to the sciatic nerve. It passes over the back of the hip joint, to which it gives an articular branch, and continues downwards deep to obturator internus and the gemelli, to sink into the anterior surface of quadratus femoris. It also supplies the inferior gemellus.
Gluteal intramuscular injection
The upper outer quadrant of the gluteal region is a common site for intramuscular injections. To avoid damage to the sciatic nerve it must be noted that the gluteal region extends from the iliac crest to the gluteal fold. In the above quadrant the needle enters gluteus medius or gluteus maximus, depending on the exact position chosen.
Hip joint
The hip joint is a multiaxial synovial joint of the ball-and-socket variety, between the acetabulum of the innominate (hip) bone (Fig. 3.48) and the head of the femur (Fig. 3.50). In general it can be said that in all joints stability and range of movement are in inverse proportion to each other; the hip joint provides a remarkable example of a high degree of both. Its stability is largely the result of the adaptation of the acetabulum and femoral head to each other, and its great range of mobility results from the femur having a long neck that is much narrower than the head.
The cup-shaped acetabulum is formed by fusion of the three components of the hip bone: ilium, ischium, and pubis. The articular surface, covered with hyaline cartilage, does not occupy the whole of the acetabular fossa, but is a C-shaped concavity that is broadest above, where the body weight is transmitted in the erect posture. Its peripheral edge is deepened by a rim of fibrocartilage—the acetabular labrum—which encloses the femoral head beyond its equator, thus increasing the stability of the joint. The labrum is triangular in section, with its base attached to the acetabular rim. It is continued across the acetabular notch at the inferior margin of the acetabulum as the transverse ligament. The central non-articular part of the acetabulum is occupied by a pad of fat (the Haversian pad).
The spherical head of the femur is covered with hyaline cartilage. The non-articulating summit of the head is excavated into a pit (fovea) for attachment of the ligament of the head of the femur (ligamentum teres), whose other end is attached to the transverse ligament and the margins of the acetabular notch.
The capsule of the joint is attached circumferentially around the labrum and transverse ligament, whence it passes laterally, like a sleeve, to be attached to the neck of the femur. In front it is attached to the intertrochanteric line, but at the back it extends for only half this distance, being attached halfway along the femoral neck (Fig. 3.12). The capsule is loose but extremely strong.
From these attachments the fibres of the capsule are reflected back along the neck of the femur to the articular margin of the femoral head. This reflected part constitutes the retinacular fibres, which bind down the nutrient arteries that pass, chiefly from the trochanteric anastomosis, along the neck of the femur to supply the major part of the head. Fracture of the femoral neck within the capsular attachment ruptures the retinacular fibres and the vessels, causing avascular necrosis of the head.
The fibrous capsule is strengthened by three ligaments, which arise one from each constituent bone of the hip bone.
The iliofemoral ligament (of Bigelow) is the strongest of the three, and has a triangular shape (Fig. 3.14A). The apex is attached to the lower half of the anterior inferior iliac spine and the base is attached to the intertrochanteric line. The margins are thick and the ligament has the appearance of an inverted V (though often being referred to as the Y-shaped ligament). The ligament limits extension at the hip joint.
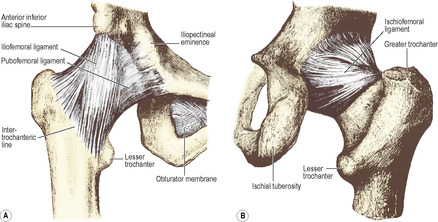 |
| Figure 3.14 |
The pubofemoral ligament is attached to the superior ramus and obturator crest of the pubic bone. It passes distally deep to the iliofemoral ligament, and blends with the capsule (Fig. 3.14A).
The ischiofemoral ligament is the weakest of the three. It arises from the posteroinferior margin of the acetabulum, and its fibres, passing laterally to the capsule, spiral upwards and blend with circular fibres of the capsule, the zona orbicularis (Fig. 3.14B). The zona is responsible for the hourglass constriction of a normal arthrogram.
As in all synovial joints, the synovial membrane is attached to the articular margins. From its attachment around the labrum and transverse ligament it lines all the capsule and is reflected back along the neck of the femur, where it invests the retinacular fibres up to the articular margin of the head of the femur. The Haversian fat pad and the ligament of the head are likewise invested in a sleeve of synovial membrane that is attached to the articular margins of the concavity of the acetabulum and of the fovea on the femoral head. Occasionally (10%) a perforation in the anterior part of the capsule, between the iliofemoral and pubofemoral ligaments, permits communication between the synovial cavity and the iliac bursa.
Relations
Anteriorly the psoas major tendon separates the capsule from the femoral artery and more medially pectineus intervenes between the capsule and the femoral vein. The femoral nerve lies lateral to the artery in a groove between iliacus and the psoas tendon. Iliacus is partly separated from the capsule by the bursa. Superiorly the reflected head of rectus femoris (medially) and gluteus minimus (laterally) are in contact with the capsule. Inferiorly obturator externus spirals below the capsule to the back of the femoral neck. Posteriorly lies piriformis, and below it the obturator internus tendon and the gemelli separate the sciatic nerve from the capsule. Laterally the capsule blends with the iliotibial tract. Medially the floor of the acetabular fossa forms part of the lateral wall of the pelvis, and in the female the ovary lies adjacent, separated only by obturator internus, the obturator nerve and vessels and the peritoneum.
Blood supply
The capsule and synovial membrane are supplied from nearby vessels. The head and intracapsular part of the neck receive their blood from the trochanteric anastomosis (see p. 126), mainly through branches of the medial circumflex femoral artery. Although the artery in the ligament of the head of the femur (from the obturator artery) is important in the young child, it is usually considered to have atrophied by the age of about 7 years (but bleeding from it at adult hip operations suggests that it may often remain patent for much longer).
Nerve supply
The femoral nerve via the nerve to rectus femoris, the obturator nerve directly from its anterior division, the nerve to quadratus femoris and articular twigs from the sciatic nerve all supply the hip joint. The femoral, obturator and sciatic nerves also supply the knee joint (see p. 140), and pain arising in the hip joint may be referred to the knee.
Movements
As in any ball and socket joint, movement is possible in all directions. Flexion, extension, adduction and abduction are free; a combination of all four produces circumduction. In addition, medial and lateral rotation of the femur occur.
In flexion of the hip the head of the femur rotates about a transverse axis that passes through both acetabula (Fig. 3.15) and the thigh is flexed upon the trunk. The muscles responsible for flexion are psoas major and iliacus, assisted by rectus femoris, sartorius and pectineus. Flexion is limited by the thigh touching the abdomen, or by tension of the hamstrings if the knee is extended; the normal range is about 120°, with the knee flexed.
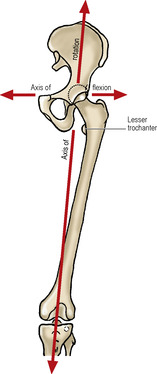 |
| Figure 3.15 |
Extension of the thigh, the reverse of the above movement, is performed by gluteus maximus at the extremes of the movement and by the hamstrings in the intermediate stage. The movement is limited by tension in the iliofemoral ligament, and amounts to about 20°.
In adduction and abduction of the thigh the femoral head rotates in the acetabulum about an anteroposterior axis. Adduction of about 30° is produced by contraction of the pectineus, adductors longus, brevis and magnus and the gracilis. It is limited by contact with the other leg or, if the latter is abducted out of the way, by the tension of gluteus medius and minimus. Abduction is produced by contraction of gluteus medius and minimus, assisted by tensor fasciae latae and sartorius. It is limited by tension in the adductors and in the pubofemoral ligament, and amounts to about 60°. Contraction of the abductors is essential in normal one-legged stance and in walking and running (see p. 125). In the sitting position, piriformis and the gemelli and obturator muscles act as abductors, e.g. helping to move the leading leg when getting out of a car.
In rotation the femoral head rotates in the acetabulum about a vertical axis that passes through the centre of the femoral head (Fig. 3.15). On account of the angulation of the neck of the femur, this axis does not coincide with the axis of the femoral shaft. Consequently the femoral neck and greater trochanter move forwards during medial rotation, and backwards during lateral rotation.
Medial rotation is produced by the anterior fibres of gluteus medius and minimus assisted by tensor fasciae latae. It is restricted by tension in the lateral rotators and the ischiofemoral ligament. Pyriformis, obturator internus and the gemelli, quadratus femoris and obturator externus are lateral rotators, assisted by gluteus maximus and sartorius. Lateral rotation is restricted by tension in the medial rotators and the iliofemoral ligament. Rotation in either direction amounts to about 40°.
If the neck of the femur is fractured, the shaft is free to rotate about its own axis, and psoas and iliacus produce the lateral rotation of the limb that is the characteristic feature of a fractured femoral neck.
Stability
The snug fit of the femoral head into the acetabulum, deepened by the labrum, makes the hip a very stable joint, further reinforced by the ligaments on the outside of the capsule, especially the iliofemoral. The short muscles of the gluteal region are important muscular stabilizers. The joint is least stable when flexed and adducted; dislocation requires considerable force but may occur, for example, in serious car accidents; the head of the femur is typically displaced posteriorly and there is often an associated fracture at the back of the acetabulum. Acetabular dysplasia, ligamentous laxity and intrauterine malposition are contributory factors for congenital dislocation of the hip in about 1.5 per 1000 live births; there are genetic variations in this incidence. Girls are more often affected than boys and the condition may be bilateral. The femoral head dislocates posteriorly and comes to lie on the gluteal surface of the ileum.
Surgical approach
The hip joint can be approached from the front, side or back. From the front and side the routes lie in front of, through or behind tensor fasciae latae. The anterior approach is through the interval between sartorius and tensor fasciae latae, detaching the tensor, rectus femoris and the anterior part of gluteus minimus from the ilium so that the upper and anterior parts of the joint capsule can be reached. The anterolateral approach is between tensor fasciae latae and gluteus medius, exposing the capsule by retracting the anterior borders of gluteus medius and minimus or by detaching their insertion by performing an osteotomy of the greater trochanter. The ascending branches of the lateral circumflex femoral vessels are a source of bleeding during this approach, and the superior gluteal nerve is at risk at the upper end of the exposure. The posterior approach involves splitting the middle of gluteus maximus in the line of its fibres. Piriformis, obturator internus and the gemelli are divided at their femoral attachments to display the capsule. The sciatic nerve is retracted medially and is protected by turning the cut ends of obturator internus and the gemelli backwards over the nerve.
Injection or aspiration of the joint can be carried out from the front or side. At the front the needle is inserted 5cm below the anterior inferior iliac spine and 4 cm lateral to the femoral pulse and directed upwards, backwards and medially. For the lateral approach the needle passes in front of the greater trochanter and parallel with the femoral neck, entering the capsule through the lower ends of gluteus medius and minimus.
Part four. Posterior compartment of the thigh
The posterior or hamstring compartment of the thigh extends from the buttock to the back of the knee. It is separated from the anterior compartment by the lateral intermuscular septum, but there is no septum dividing it from the medial or adductor compartment, for the adductor magnus is a muscle consisting of fused adductor and hamstring components.
The cutaneous nerve supply is by the posterior femoral cutaneous nerve, which runs vertically downwards deep to the fascia lata, pierces it behind the knee, and ends halfway down the calf. It sends branches through the fascia lata to supply the overlying skin.
Hamstring muscles
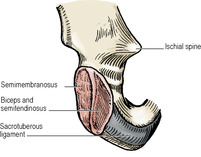
The hamstring muscles all arise from the ischial tuberosity and are inserted into the tibia or fibula; they thus span both the hip and knee joints. They are the semimembranosus, semitendinosus and biceps femoris (long head). The short head of biceps arises from the back of the femur. The hamstring part of adductor magnus is described on page 122.
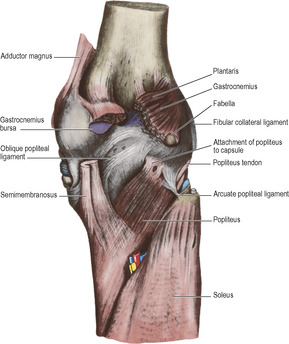
Semimembranosus
This extends from the ischial tuberosity to the medial condyle of the tibia. It arises from the lateral part of the ischial tuberosity (Fig. 3.16), above the part that bears weight in sitting. This origin is a long flat tendon, from which muscle fibres commence about mid-thigh. The distal attachment of the muscle is by a rounded tendon into the horizontal concavity on the back of the medial condyle of the tibia (Figs 3.17 and 3.19). From this insertion three expansions diverge. One passes forwards along the medial surface of the condyle deep to the tibial collateral ligament of the knee, separated from it by a bursa. A second expansion passes obliquely upwards to the lateral femoral condyle as the oblique popliteal ligament (see p. 137), while the third forms a strong fascia overlying popliteus and reaches the soleal line of the tibia.
 |
| Figure 3.16 |
Semitendinosus
This arises, in common with the long head of biceps, from the medial part of the ischial tuberosity (Fig. 3.16). The fleshy belly diminishes in size from above downwards to a cord-like tendon that lies on the posterior surface of the muscular belly of semimembranosus (Fig. 3.17). The tendon of semitendinosus passes behind the medial condyle of the femur and then curves forwards to be inserted behind gracilis into the upper part of the medial surface of the shaft of the tibia.
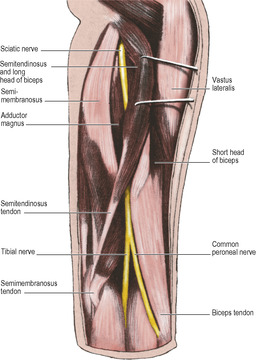
Biceps femoris
This muscle has two heads of origin. The long head arises, in common with semitendinosus, from the ischial tuberosity (Fig. 3.16). It passes downwards and laterally, crossing the sciatic nerve on its posterior aspect, and joins the short head which has a long origin, from the whole length of the linea aspera and the upper part of the lateral supracondylar line of the femur (Fig. 3.50B). Distally the single tendon of the muscle is folded or split around the fibular collateral ligament of the knee joint and is inserted into the head of the fibula (Fig. 3.26).
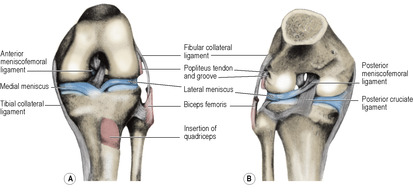 |
| Figure 3.26 |
Blood supply of the hamstrings. The hamstring compartment receives its blood supply mainly from the profunda femoris artery and its perforating branches. These pierce the adductor magnus and give off large branches to the hamstrings and the overlying fat and skin. The blood supply of the upper part of the hamstrings is derived from the inferior gluteal artery and that of the lower part from the popliteal artery. These and the perforating branches of the profunda femoris form a series of anastomoses along the back of the thigh. The highest is the cruciate anastomosis.
Nerve supplies. The three muscles are supplied, with the ischial part of adductor mangus, by the tibial component of the sciatic nerve (L5, S1), with the exception of the short head of biceps, which is supplied by the common peroneal (fibular) part of the sciatic nerve.
Actions. Acting from above the hamstrings flex the knee joint, and acting from below they extend the hip joint. With the knee semiflexed, biceps femoris is a lateral rotator, while semimembranosus and semitendinosus are medial rotators of the leg.
Test. While lying face downwards with the limb straight, the knee is flexed against resistance, and the tendons of biceps and semitendinosus palpated above the knee on the lateral and medial sides respectively.
Sciatic nerve
The sciatic nerve runs vertically through the hamstring compartment, lying deep to the long head of biceps, between it and the underlying adductor magnus (Fig. 3.17). At the apex of the popliteal fossa, a hand’s breadth or more above the knee joint, it divides into its tibial and common peroneal (fibular) components; but the division may occur at a higher level (see p. 127).
The surface marking of the nerve is from the midpoint between the ischial tuberosity and greater trochanter to the apex of the popliteal fossa.
Part five. Popliteal fossa and knee joint
The popliteal fossa is a diamond-shaped space behind the knee (Fig. 3.18




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree