Fig. 7.1
Flowchart of the cellular events in acute injury following sulfur mustard exposure. (Red arrow: inhibitory pathway, Dotted line: under study or possible pathway, Boxes with “lock” symbol; Steps needs more investigation)
The processes mentioned above occur in patients who are exposed to a great amount of SM. However, in slightly injured patients, the process is milder and the healing begins more rapidly. In these patients, symptoms become evident a few weeks after exposure. Nevertheless, in severely injured victims, mechanical ventilation and other respiratory supports may be required and, likewise, the treatment takes more time to produce its effects (Muskat 2008).
The late respiratory complications of SM exposure are more important, as they have a greater morbidity and mortality. In several cases, chronic symptoms may persist or reoccur after years. The most probable cause is a chronic process that this chapter will focus upon.
7.3 Mechanism of Long-Term Respiratory Complications
Bronchiolitis, bronchitis, and COPD, asthma, pulmonary fibrosis, emphysema, pneumonitis, pneumonia and interstitial lung diseases were suggested for justifying the main lower respiratory complications of the SM poisoning (Mostafa Ghanei and Amin Saburi 2011; Ghanei et al. 2008a; Ghanei and Harandi 2007; Razavi et al. 2013a; Hefazi et al. 2005). The lacks of a suitable response to specific treatments, such as corticosteroids, and also further studies have clarified the specific characteristics of these patients. Due to different and sometimes contradictory pathogenesis, the term of Mustard Lung (ML) has been suggested by Ghanei et al. to be included in the literature although there is concern about accuracy of the use of such term (Beheshti et al. 2006). Also, it seems that the patient’s clinical and paraclinical findings can be justified by diseases of the small caliber airways, such as constrictive bronchiolitis or bronchiolitis obliterans (BO) (Ghanei et al. 2008a, 2011a, b; Ghanei and Harandi 2007, 2011; Saber et al. 2012).
According to our experience and the literature, in these cases, thick sputum, chronic cough, irritable airways, recurrent upper and lower respiratory tract infections, chest tightness and dyspnea are the most common clinical features. These manifestations relate to an insufficient repair process and therefore, a chronic damage and incomplete healing in the small airways, lead to chronic secretion and injury of the epithelial layer.
Among the mentioned mechanisms of BO in the exposed cases, four mechanisms are more important, as followings:
1.
Chronic inflammation
2.
Proteolysis
3.
Lack of balance between oxidative stress and antioxidant mechanisms
4.
Apoptosis
The following section of this chapter will discuss the above mentioned mechanisms, to have an insight on the cellular and molecular processes, which would enhance the understanding of the clinical and paraclinical presentations.
7.3.1 Chronic Inflammation
Chronic inflammation is the first mechanism that takes place in the pathogenesis of SM exposure (Emad and Rezaian 1997). Different inflammatory mediators, particularly interleukin (IL) 8 and 6 play important roles in pathology of these patients (Pourfarzam et al. 2009). Emad and Rezaian (1999)., in one of the first studies on these patients, considered pulmonary fibrosis (PF) as the main morphopathological alteration of exposed lungs, making chronic inflammation as the main responsible for the PF (Emad and Rezaian 1999). They described neutrophilic alveolitis as the main feature in bronchoscopic biopsy, noting that neutrophils and eosinophil were the most frequent inflammatory cells in the bronchoalveolar lavage (BAL) specimens (Emad and Emad 2007c). These mediators (inflammatory markers such as cell count and level of ILs) are also regarded as biomarker with a strong correlation with the severity of the disease (Emad and Emad 2007c). On the other hand, these findings are similar to biological findings in COPD patients (Larsson 2008). When COPD is aggravated, IL-6 and IL-8 increase in BAL and serum samples. All inflammatory cells, which include macrophages, B and T lymphocytes and neutrophils, are increased in the alveoli and airways of patients with COPD (Ji et al. 2014). Inflammatory indices are also considered as predicting factors of disease intensity and mortality in COPD (Celli et al. 2012; Higashimoto et al. 2009).
To our experience and in congruence with previous studies, in the pathogenesis of BO, as the main sequel of SM exposure, proliferation of fibroblasts and tissue regeneration play important roles and peribronchial fibrosis can ensue (Myong et al. 2001). Different growth factors, among which transforming growth factor β (TGF-β) is the most studied, can increase the reactivity of fibroblasts and increase collagen accumulation. The excessive expression of TGF-β in macrophages and endothelial cells can be an indicator of the changes resulting from BO. The target cells of TGF-β are present in great numbers BAL samples and also target tissues of the patients exposed to SM (Aghanouri et al. 2004; Mostafa Ghanei and Amin 2011).
A research conducted on 50 chemical war victims, compared levels of high-sensitivity C-reactive protein (hs-CRP) with the control group. The pooled results showed increased levels of this protein in exposed patients and a direct relationship with the intensity of the disease (Attaran et al. 2009).
Levels of cytokines, such as IL-12, tumor necrosis factor-alpha (TNF-a), IL-6, IL-1 beta, were higher in the study group compared to their peered controls. In addition, the high level of cytokines in this study’s population was strongly correlated with fibrosis intensity (Emad and Emad 2007a; Shohrati et al. 2014a). It is necessary to note that PF was increased in the chemical victims in the pilot studies, an issue which was later debated for years.
Further studies and evidence showed that fibrosis was not an evident finding in the pulmonary pathology of these patients. In addition, although inflammation and inflammatory processes, along with the oxidative stress phenomenon play important roles in the pathology of the initial stages of exposure to SM, the interaction between these two pathologies were more studied to declare the main pathogenesis.
More recent trials have revealed that that the level of inflammatory mediators is not high in these victims, and also, for some of them, such as CRP, IL-8, IL-1 and rheumatoid factor (RF), the levels were even lower in comparison to the control groups. No correlation between IL-8 level and pulmonary symptoms was found (Pourfarzam et al. 2009). It should be noted that, although the main pathology in chemical victims is bronchiolitis, this type of bronchiolitis has major differences from the obstructive bronchiolitis, which results from pulmonary transplantation.
These differences, which were found between lung of the chemical victims and other pulmonary patients, were responsible for different and unique appearances and responses to treatment in the injured patients. The lack of a satisfactory response to corticosteroid treatment in more than 50 % of these patients is an argument for a decreased presence of active inflammation in them (Mostafa Ghanei and Amin 2011). The study, which was conducted on the samples obtained from open pulmonary biopsy of these patients, revealed only mild to moderate lymphocytic infiltration, even for the cases with a severe pathology.
7.3.2 Increase of Proteolysis
Disruption of the balance between proteolytic and anti-proteolytic molecules causes metabolic hyperactivity. The result of this phenomenon is a proteolytic destruction of the healthy cells in patients with COPD. Since emphysema was not observed in lungs of the chemical victims who did not smoke, the presence of proteolytic activity is not possible in the patients without emphysema (Ghanei et al. 2008c).
7.3.3 Oxidative Stress
There are multiple evidences on the presence of oxidative stress and oxidative intermediaries in patients with COPD. The markers relating to oxidative stress in these patients are 4–hydroxynonenal (4–HNE), hydrogen peroxide (H 2 O 2 ) and isoprostane, which are end products of lipid peroxidation. The role of oxidative factors is evident when their activity and effect overcome antioxidant factors. The result of this imbalance is damage of lipids, proteins and DNA. This cellular damage process induces apoptosis and alterations of pulmonary matrix, including elastin and collagenfibrillar structures (Sarsour et al. 2009). Oxidative stress exerts its effect by inactivating antiproteases, such as alpha–1 antitrypsin (AAT) or leukoprotease secretion inhibitors, or activating metalloproteinase oxidants. Oxidants play a major role in the inflammatory damage of lungs, inducing the translation of proinflammatory genes (Demedts et al. 2006).
To study oxidative stress in chemical victims, the levels of glutathione (GSH) and malondialdehyde (MDA) have been measured. Results have shown that the victims with moderate to severe pulmonary damage had lower levels of GSH and a higher rate of MDA. An increase of MDA indicates the increase of lipid peroxidation, which is a consequence of the production of free radicals after exposure to SM. Nevertheless, the reduction of GSH levels is not only limited to pulmonary patients exposed to MS, as its levels decrease when they are exposed to other airborne toxins, such as ozone and tobacco (Fidan et al. 2005; Shohrati et al. 2010a).
Several studies have been conducted on the effect of apolipoprotein A1 (APOA1) and S100 calcium binding protein family. High levels of these proteins indicate a lack of balance between oxidant and antioxidant substances in chemical victims. Dr. Mehrani et al., using a proteomic method, tried to identify different proteins expressed in these victims, compared with healthy people. Results showed that there was APOA1 in all BAL samples of patients exposed to SM, while none of the healthy volunteers showed such protein. A direct relationship between the intensity of pulmonary disease and APOA1 and isoform haptoglobin was also noted. The S100 protein was also found in all patients who had moderate to severe pulmonary damage (Mehrani et al. 2009; Mostafa Ghanei and Amin 2011).
7.3.4 Apoptosis
New information indicates the important role of apoptosis in the pulmonary pathology of SM victims. It is necessary to note that two main pathways play a crucial role in apoptosis, and they are termed the intrinsic apoptotic pathway and extrinsic apoptotic pathway (Saburi et al. 2012a; Mostafa Ghanei and Amin 2011). It is necessary to note that apoptosis is not an isolated process, also occurring in COPD pathogenesis, while other pathways, such as those of the oxidative stress, increase the complexity of this process. Apoptosis is recognized as a method of cleaning performed by neutrophils, classically evident in the process of inflammation. Wherever there is oxidative stress in lungs, apoptosis will ensue. This indicates a positive relationship between these two phenomena (Tse and Tseng 2014).
On the other hand, “efferocytosis” is a process in which the cells that have apoptosis are cleaned by phagocytes (Simpson et al. 2013). If this is not done, the apoptosed neutrophils will be a new inductive factor for oxidative stress. The efficiency of efferocytosis has been suppressed by oxidants and while antioxidants increases it (Simpson et al. 2013; Lee and Surh 2013; McPhillips et al. 2007). Tumoral growth factor-beta (TGF-β) is one of the substances that have a relationship with efferocytosis. Zarin et al. in their study stated that “TGF-beta1 and TGF-beta3, but not TGF-beta2, secretion is a result of efficient efferocytosis in chemically injured patients, playing a protective role by improving airway remodeling and lung homeostasis in this group” (Zarin et al. 2010). Deficiency in efferocytosis is encountered in multiple pulmonary diseases, such as asthma and COPD. In vivo and in vitro studies have proved the presence of apoptosis as one of the main cause’s involved in pulmonary damage in chemical victims. It was shown that both the intrinsic and extrinsic apoptotic pathways are active in lungs of chemical victims (Tang and Loke 2012; Saburi and Ghanei 2013). It has been shown that different types of translations relating to TGF-β and high levels of the TGF-β protein are present in the BAL of the chemical victims, being measurable with ELISA method. It has been concluded that TGF-β may be responsible for the regeneration of airways, hemostasis and slow progress of disease in chemical victims. As a result, it has been suggested that TGF-β1 and TGF-β3 may improve efferocytosis and play important roles in the regeneration of the airways of these patients. These capabilities of TGF-β are promoters of prolonged life in these patients, compared with the patients with BO resulting from lung transplantation (Jonigk et al. 2010; Zarin et al. 2010).
As mentioned above, low levels of GSH is also an important factor for induction of apoptosis in the chemical victims. Rosenthal et al. have shown the role of caspase activity in the apoptosis of these patients and the early light-inducible protein (ELIP), which is a protein similar to caspase-8, is affected after exposure of pulmonary cells to low concentration of SM (Rosenthal et al. 2003; Saburi and Ghanei 2013; Saburi et al. 2012b).
Complementary studies indicated that the phenomenon of apoptosis in chemical victims is not performed completely. For example, in the injured patients and control group, the caspase-3 level did not record considerable differences although there are some contradictions (Pohanka et al. 2013; Pirzad et al. 2010). More analysis of lung lavage fluid with annexinV-fluorescein isothiocyanate (FITC) kits proved that the majority of the cells had necrosis and only few of them had completed the phenomenon of apoptosis (Keyser et al. 2013). The homeostasis of calcium and S100 protein are reduced in these patients, while the two play pivotal roles in the regulation of apoptosis and regeneration of tissues (Mehrani et al. 2009). Figure 7.2 shows the suggested mechanisms of the long-term lung complications of SM.
Fig. 7.2
Flow chart of the suggested mechanisms of the long-term lung complications of SM (Published in Critical Review in Toxicology, Informa Healthcare, with permission)
Recently, accumulation of IL-17(+) cells in the injured areas of the lungs has been suggested as the responsible reason of the lung squeal in chronic phase (Mishra et al. 2012). This cell can affect all four aspects which were discussed above. If a mutation would be found in this cell genome, it can be a new horizon for research to find the mechanism of the Mustard Lung.
7.4 Clinical and Pathological Findings and the Relationships with the Bronchiolitis Obliterans Mechanisms
Inhalation of SM can create different degrees of pulmonary diseases. Although the previous studies have reported affliction with pulmonary fibrosis (PF) after exposure to SM, our studies on the clinical and radiological manifestations of patients who were permanently injured by SM exposure specified that PF was not the dominant pathological pattern. Based on complementary reports, PF was the least important pulmonary change in patients (Taghaddosinejad et al. 2011; Saber et al. 2012; Hefazi et al. 2005). It is not clear if this disease presents with interstitial pneumonia, similar to other interstitial pneumonia diseases, or has unclear clinical signs. The pooled results are general and include parenchymal injuries and airways mucous damages (Veress et al. 2010).
In novel studies based on High Resolution Computed Tomography (HRCT), air trapping has been reported as the prevalent finding, which indicates the presence of BO as the underlying disease (Ghanei et al. 2004b; Idani et al. 2012). Ghanei et al. at their research demonstrated that “the most frequent findings were; air trapping 38 (76 %), bronchiectasis 37 (74 %), mosaic parenchymal attenuation (MPA) 36 (72 %), irregular and dilated major airways 33 (66 %) bronchial wall thickening (BWT) 45 (90 %), and interlobular septal wall thickening (SWT) 13 (26 %)” (Ghanei et al. 2004b) (Figs. 7.3 and 7.4).
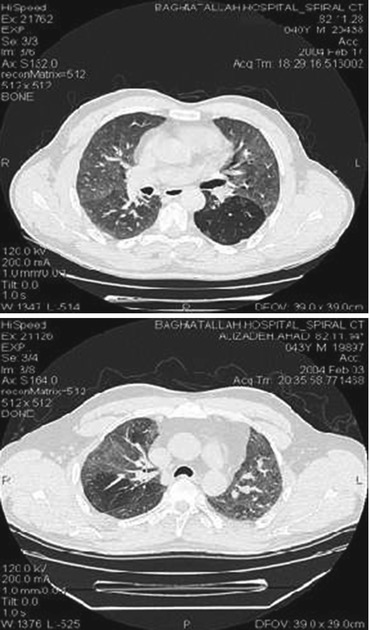
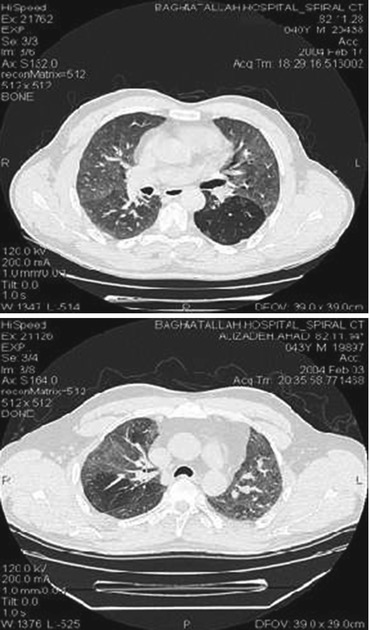
Figs. 7.3 and 7.4
HRCT findings in chemical injured cases. Air trapping, mosaic pattern and centri lobular emphysema are the most common findings (Authors captured, published in Resaneh Takhasosi Publication, Iran, with permission, Mostafa Ghanei (2011))
To study BO and pulmonary air trapping in patients, HRCT should be performed at the end of the exhalation phase, because obstruction in bronchioles is a cause of air trapping and this state is observed during exhalation. Pulmonary air trapping of more than 25 % on HRCT strongly indicates BO (Ghanei et al. 2004b). Mosaic perfusion in BO results from hyperaeration of terminal alveoli to bronchioles due to obstruction in proximal. On the other hand, the presence of areas with low blood perfusion and non-engaged areas with normal perfusion or increased perfusion create the mosaic pattern due to contraction of vessels, as visible on HRCT. Although patients were not in a hyper aeration stage, the mosaic pattern was found on HRCT. In the spirometry of these patients, obstructive, restrictive or sometimes normal pattern was reported (Leung et al. 1998; Ghanei et al. 2010a).
In study of these patients, it was specified that there were not provided sufficient tissue samples to differentiate the type of bronchiolitis after sampling by needle biopsy or in the samples prepared with transbronchial method. The reported pathology in these cases was organizing pneumonia and in cases where opening sampling of lung tissues was performed or tissue sampling was prepared by Video Assisted Trachoscopy (VAT), BO diagnosis was confirmed. The bronchoscopic biopsy is an accepted technique for the diagnosis and follow-up of patients with organizing pneumonia (Beheshti et al. 2006; Mostafa Ghanei and Amin 2011). In our study on the histology of patients exposed to SM with bronchoscopic biopsy, damage to the tracheobronchial tree, base membrane, edema, infiltration of mononuclear cells into the lamina propria, fibrosis of lamina propria and muscular mucous hyperplasia were found. These structural changes may indicate a chronic reaction following the inhalation of SM (Beheshti et al. 2006; Ghanei et al. 2011a; Ghanei and Harandi 2011).
7.5 Changes of Respiratory Ducts Due to SM
The extent of the changes in the respiratory ducts following contact with SM depends on the duration of contact and the concentration of the chemical in the inhaled air. In hot climatic conditions, the effects of hot SM on the respiratory system are intensified. The findings obtained during the First World War are hardly interpretable, due to the high incidence of secondary infections in the studied samples after death (Lewisite 1993).
In case of intensive contact and during the acute phase, the epithelial layers of the larynx, lung and bronchi are necrosed and even pseudomembrane formation occurs. In cases of contact with lower intensity, petechiae are prevalent on surface layers of respiratory ducts. Similar injuries were also found in respiratory ducts of tested animals, several months after contact with SM (Balali-Mood and Hefazi 2006; Karacsonyi et al. 2009). During the First World War, severe conditions, such as gangrenous changes, were found in lungs. In a study with the optical microscope, the epithelial secretions of fibrin and mucous cells were intense (Lewisite 1993). In this report, the base membrane was altered due to swelling and occurrence of edema in epithelial tissues, along with infiltration of inflammatory cells and dilation of blood vessels was a usual finding (Mostafa Ghanei and Amin 2011).
In more intensive cases of contact, injuries are expanded to the connective tissues and smooth muscles of the wall of respiratory duct. During the healing stage, the extensive metaplasia of the squamous epithelial cells and the first changes were also visible in mucous glands ducts (Ghanei et al. 2006b). The laminated metaplastic squamous epithelial cells completely cover surfaces of the injured regions (Lewisite 1993).
In these studies, the growth stages of these epithelial cells were not well described, while the settlement of the pseudostratified columnar cells was not evident in the epithelial layer.
7.6 Tracheobronchomalacia and Air Trapping After SM Exposure
One of the side effects of SM in chemical victims is Tracheobronchomalacia. Tracheobronchomalacia and air trapping are found in the thoracic HRCT of nearly all patients exposed to SM (Ghanei et al. 2006a).
The findings of our studies first showed that air trapping and Tracheobronchomalacia were related to each other, as long-term side effects of SM exposure. The accompaniment of air trapping and BO is induced by a main single process, which generates air trapping in large and small airways in these patients. The intensive stricture of tracheobronchial tree has been reported in several of these cases. Tracheobronchomalacia is usually diagnosed by HRCT, while at present its standard global diagnostic method is bronchoscopy (Ghanei et al. 2006a).
Given that air trapping is a more prevalent finding than tracheobronchomalacia in the chemical victims, it can be concluded that air trapping is not the outcome of Tracheobronchomalacia in this group, while similar pathological mechanisms, which leads to small airways disease, i.e. BO, may lead to disruption of large airways such as in the case of tracheobronchomalacia. In other words, SM may affect epithelium of both small and large airways.
7.7 Sign and Symptoms
7.7.1 Symptoms in Acute Phase
The major characteristic of contact with SM is the occurrence of a period without clinical signs and symptoms, several hours after contact. Duration of this period depends on contact, ambient temperature and individual characteristics. Some people show a superior sensitivity to SM compared with others. At time of chemical injury, airways, eyes and skin are directly exposed to SM and clinical symptoms appear at their level. Nevertheless, in case it is absorbed in a high amount by lung or skin tissues, it can induce complications in the circulatory, digestive and central nerve system (Razavi et al. 2013a).
At initial minutes (20–60 min) after exposure, coughing, shortness of breath, nausea, vomiting, eye pain (shooting pain) is sometimes found but symptoms may often be absent. After some hours, fatigue, periorbital edema, intensive eye pain, tears, skin erythema, and minor respiratory symptoms (e.g. coughing, shortness of breath, rhinitis, sneezing, epistaxis, and hoarseness of voice) are clear. After 24 h, vesicles become more evident and more considerable symptoms of respiratory appear (Mostafa Ghanei and Amin 2011; Marrs and Al 2007).
7.7.2 Late Symptoms
The eyes, skin and respiratory system are the organs that are affected primarily and secondarily by the poisonous action of this substance. The skin and eye lesions may persist on the long-term or can be reduced. However, pulmonary complications are the most prevalent delayed conditions of these patients, and they can progress over time (Khateri et al. 2003). The effect of SM is affected by different factors. Exposure intensity is so high that symptoms of the person at time of exposure reflect it. Nonetheless, it should be noted that environmental factors and genetic factors can change the organic response to SM (Hosseini-Khalili et al. 2008; Taravati et al. 2013).
Different studies indicate that the intensity of primary symptoms resulting from SM exposure relates to the risk of pulmonary obstructive diseases. Patients with primary weak symptomatology have a lower risk of obstructive diseases compared to the patients with moderate to severe primary symptoms (Mostafa Ghanei 2011). The pulmonary obstructive pattern is the most prevalent in the pulmonary function test (PFT) after exposure to SM and does not have a relationship with moderate to severe primary symptoms of the patients. In the patients who had mild to moderate pulmonary symptoms after exposure, pulmonary function was normal and they have had less pulmonary secondary pattern over time. It seems that, in case the intensity of SM exposure induces primary symptoms and the hospitalization of the person at time of exposure, the incidence of the late pulmonary complications will be augmented (Ghanei et al. 2008a). However, changes in symptom intensity from moderate to severe or periodical hospitalization in the hospital after exposure do not lead to changes of the symptoms. Therefore, it seems that other factors, such as personal susceptibility to the intensity of the primary symptoms and hospitalization probability are more valuable (Mostafa Ghanei and Amin 2011).
Findings in patients presenting with the chronic phase have no relationship with premature pulmonary symptoms. Our findings indicate that the increase of premature pulmonary symptoms intensity does not correlated with air trapping or mosaic diffusion. These two findings have been found in radiographic images of symptomatic and asymptomatic exposed people. As mentioned before, histopathological studies and radiological findings (HRCT) support the diagnosis of BO in SM exposed victims (Ghanei et al. 2011a; Kehe et al. 2008).
7.7.3 Chronic Coughing
Regarding the SM victims who suffered from BO, our study showed that the aforementioned causes influenced the incidence of coughing and intensity of chronic coughing in patients exposed to SM. The conducted studies show that the principal reason for chronic coughing in SM exposed victims was the contraction of bronchus, and therefore, it imposes the necessity to study them and prescribe adequate treatment when available (Ghanei et al. 2005a, 2006c).
The importance of this issue, particularly in patients exposed to SM, increases when we compare the results of our study with the unexposed people. More than 90 % of the studied patients had a combination of chronic coughing causes. Therefore, it can be concluded that, despite the known causes of chronic coughing in patients exposed to SM, each patient with chronic bronchitis induced by SM should be evaluated more thoroughly for other causes of chronic coughing, particularly in uncontrolled chronic coughing or recently intensified coughing. In addition, since the number of related causes in SM exposed patients is considerably higher than in the non-injured population, it is suggested to study potential exposure to mustard gas when the patients have chronic coughing induced by different factors.
It should be emphasized that chronic coughing in chemical victims should not be attributed only to SM exposure, and other causes of coughing such as gastro esophageal reflux should also be considered, because coughing cannot be cured properly in the absence of a clear diagnosis (Karbasi et al. 2013).
7.8 Incidence and Diagnosis of Emphysema in SM Victims
Emphysema is morphologically defined as resistant enlargement of distal airways up to the level of the terminal bronchiole and destruction of its walls without evident fibrosis. Age and smoking are several of its main causes. Deficiency of AAT enzyme is a genetic factor, which can lead to premature installation of emphysema. The main methods used for identification of emphysema are PFT and chest radiology. Although these methods are not sensitive enough for early identification of functional and apparent abnormalities of airways, they are used in practice for apparent evaluation of the extent and intensity of HRCT diagnosed emphysema changes (Shohrati et al. 2010b).
In a case–control study, which was conducted on 20 smokers with low exposure to SM and 20 smokers without exposure to SM, PFT and chest HRCT were conducted on all participants for identification of emphysema. Sensitivity, specificity, and negative predictive value were calculated for PFT. In the group with low exposure to SM, spirometry was not able to diagnose emphysema, while chest HRCT identified parenchyma changes in five patients. In the smoking group, 11 out of 20 persons (55 %) had emphysema, as compared to the low exposure SM group, where only 5 out of 20 cases (20 %) were diagnosed with emphysema (Ghanei et al. 2007a, b). There was no case of deficiency of AAT enzyme in all 40 people (Shohrati et al. 2010b). It can be concluded that, in the people who had a record of exposure to SM, cigar can induce emphysema in younger ages. In this group, HRCT is more useful than the PFT for early diagnosis, as the PFTs were reported normal in this group.
In our studies, there was no relationship found between air trapping in HRCT and results of PFT. Pulmonary function test may not accurately identify longitudinal changes in acinar structures, which are induced by specific factors, such as age and smoking. When there is an additional pulmonary risk factor, as in the case of poisonous gas exposure, symptoms of the disease, incidence and diagnostic approach may differ from other patients. Considering the high incidence of such exposure in cities and industries, it seems necessary to study emphysema in the patients with more than one risk factor (Ghanei et al. 2007a, b).
In another study, the results of PFT were compared with HRCT findings of chest in symptomatic smokers, with or without SM exposure, after studying the incidence of emphysema and accuracy of PFT in smokers with a record of SM exposure. Results showed that the Tiffeneau index − forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC), was not a good criterion for the diagnosis of emphysema in the SM exposed group, while chest HRCT confirmed the diagnosis in five patients. In smoking patients, FEV1/FVC showed 100 % sensitivity for COPD. The FEV1/FVC results show values that are more abnormal in the smoking group than in the SM exposed group. On the other hand, chest HRCT results indicate a higher rate of emphysema in the smoking group (Ghanei et al. 2007a, b, 2008b).
In summary, smokers with additional risk factors, such as exposure to respiratory poisons, present the occurrence of emphysema at younger ages and, in this stage, spirometry is also normal. Chest HRCT should be considered as a suitable tool for early diagnosis of emphysema in smokers with exposure to poisonous gases. This additional risk factor can intensify the symptoms during the initial stages. Considering the mentioned evidence, it seems that an early diagnosis of emphysema, before installation of symptoms, is possible (Ghanei 2011).
7.9 Other Damages to Airways and Lung Parenchyma
The SM damages the mucous layer of airways, depending on the inhalation exposure rate. This damage starts from the upper airways and reaches smaller and terminal airways in case of increasing inhalation dose. The intensity of the inflammatory reaction varies from mild to severe, and induces respiratory epithelium necrosis. Pulmonary damage is present under different forms, such as acute inflammation of upper and lower air ways, secretion from upper parts of respiratory system, inflammatory exudates and formation of pseudo membrane in the tracheobronchial tree. These damages are slowly intensified within several days. Primary bronchitis is usually noninfectious. The increase of leukocytes, fever and pulmonary infiltrations are found on radiographic a imagery. This process occurs in the first 3–4 days and secondary infection ensues after 4–6 days. A daily study of the mucosa with gram staining and culture should be conducted (Anderson et al. 1996; Fatal Exposure to Mustard Gas).
In a study investigating the chronic pulmonary complication induced by SM exposure on 50 soldiers, 80 % of them had obvious abnormalities on chest radiographs and while an increase in the thickness of bronchial wall was present in all (100 %), and changes suggesting interstitial pulmonary disease (80 %) and bronchiectasis (26 %) were visible on HRCT lung scan (Bagheri et al. 2003). The aforementioned study was compared with a separate study, in which 220 persons were exposed to SM. Almost all people who had obstructive phenomena had symptoms such as coughing, asthma and degrees of pulmonary obstruction, wheezing and dyspnea (67 %), Hemoptysis (2.7 %) and respiratory distress with respiratory accessory muscles (1.8 %) (Bagheri et al. 2003).
7.9.1 Ventilation and Perfusion Disorder
As mentioned above, accumulation of secretions in airways leads to obstruction. Obstruction causes oxygen not to enter lung alveoli and carbon dioxide (CO2) induced by cell metabolism not to exit from the lung. As a result, a type of hypoventilation occurs during which PaCO2 increases and PaO2 decreases. At the same time, it has been found in animal studies that the respiratory rate decreases following inhalation of a high dose of SM. This bradypnea can intensify the hypoventilation disorder resulting from bronchus obstruction (Vijayaraghavan 1997; Shohrati et al. 2012).
7.9.2 Hemoptysis
In the acute stage of SM poisoning, mucous bleeding is present, alongside inflammation and severe injury of epithelium. In the case of excessive bleeding, it can lead to airways obstruction in conjunction with the lung lesions inducing choking of the patient. In chronic phase, hemoptysis can be due to new vascular proliferation and chronic inflammation in these cases and it is not a reliable index for lung malignancy (Ghanei et al. 2006b; Karami et al. 2011).
7.9.3 Biochemical Disorders of Lung
Increases of gamma-glutamyl-transpeptidase (GGT) activity indicate bronchus epithelium damage, while LDH activity and increased concentration of proteins indicate cytotoxic processes in lungs, resulting in damage of the epithelium of bronchi (Foy and Schatz 2004).
The evolution of these destructive processes can be stopped by excluding the induction factor. However, in particular cases, the lysis continues, accounting for tissue destruction on the long-term (Biljak et al. 2013).
7.10 Para-clinical Findings
7.10.1 Radiologic Data
In diagnosis, treatment, follow-up and evaluation of the response to treatment in chemical victims, radiological findings are very useful. For radiological study, chest X-ray (CXR) and or high resolution computed tomography (HRCT) can be used.
7.10.1.1 Chest X-Ray
Radiological findings of the thorax in chemical victims are different between the symptomatic acute condition and asymptomatic condition. Therefore, it is very important to diagnose and interpret radiographical imagery in chemical victims in different conditions. In this instance, we describe radiographical findings in pulmonary symptomatic and asymptomatic patients.
In studies conducted on CXR among these patients, there was no mass or nodule, while the X-ray was considered normal in 70 % of the cases. The most prevalent abnormal radiological pattern was the infiltration surrounding bronchus in 34 % of the patients and the increase in thickness of the bronchial wall and increase in vascular marking. In 5 % of the cases, there was an increase in the thickness of pleura. These particular findings indicate that the patients suffer from respiratory problems despite normality of CXR. Therefore, radiography is not a reliable tool for the diagnosis and evaluation of lesions among these patients (Mansoor Ghanaei and Alizadeh 1999; Razavi et al. 2013a).
Although the study of chemical victims in the secondary stage showed that most of these patients (70 %) did not had abnormal findings on CXR despite respiratory problems, however, changes of chronic bronchitis (15 %), reticular marking (9 %) and bronchiectasis (6 %) were visible (Ghanei and Harandi 2010a).
In another study, CXR findings among the chemical victims reported emphysema (26 %), increase in pleural thickness (40 %), bronchiectasis (15 %), and pneumatic infiltration (83 %). Although BO is the most clinicopatholic complication, it could not be diagnosed by CXR (Amini and Oghabian 2013).
Considering the mentioned facts, it can be concluded that the most prevalent finding of radiography is normality of lungs, and therefore, a normal X-ray does not exclude pulmonary damage in chemical victims and more investigations should be conducted, especially with HRCT, in case of suspicious diagnosis of pulmonary complication in these patients.
7.10.1.2 Lung HRCT in Patients Without Symptoms
In a study on the people who attended the SM contaminated areas for a week during which they did not had any early symptom of SM exposure, it was shown that these individuals will suffer from complications induced by SM exposure in future. The start of clinical symptoms varied from 2–3 years after attendance in the SM contaminated areas. In the HRCT of 38 % of these patients, no positive finding was found. In other 38 % of them, there was only air trapping on HRCT In addition, there was an increase of the thickness of the bronchus wall in 14.7 % bronchiectasis in 8.8 % of them and mosaic pattern in one patient. It should be noted that the presence of air trapping in more than 25 % of the patients was considered as the most sensitive and accurate finding indicating BO (Ghanei 2011).
In study by Dr. Bagheri et al., HRCT was used on 50 patients to study pulmonary changes induced after SM exposure, and the results were compared with clinical and chest radiography findings in the same patients. In all of these cases, HRCT was abnormal, while CXR was abnormal only in 80 % of them. Increases of bronchus wall thickness were reported as the most prevalent positive finding of HRCT (100 %). Other positive radiography characteristics were interstitial lung disease (ILD) (80 %), bronchiectasis (26 %) and emphysema (24 %). There was no statistically significant relationship between CXR findings and intensity of pulmonary lesions intensity. In addition, the people who had normal radiography (20 %) showed increased thickness of bronchus wall and interstitial lung disease (with lower rate), which were reported in HRCT. Based on the results of this study, the researchers concluded that an increase of thickness of bronchus wall, ILD and emphysema were the most prevalent radiological findings in these patients. For this reason, HRCT was suggested as the best radiological diagnostic tools for these patients (Bagheri et al. 2003).
In the study by Dr. Hosseini and Balali-Mood (1998), bronchography was performed in 11 individuals while HRCT was performed in 50 individuals to study a total of 61 SM exposed patients, in the secondary stage, in which most of them (81 %) had abnormal parameters in spirometry and pulmonary disease symptoms. Bronchiectasis pattern on HRCT is found. The diagnosis of bronchiectasis had been performed by bronchography in three patients and by HRCT in 13 patients. The involvement of the lower lobes was higher, compared to the upper lobes (ten versus four cases). There was no right middle lobes involvement. Although most patients did not presented bronchiectasis in CXR, there were 12 cases of bronchiectasis (24 %) and they showed a particularly bilateral involvement (Hosseini and Balali-Mood 1998).
In our study in 2004, we found that “The most frequent findings were; air trapping 38 (76 %), bronchiectasis 37 (74 %), mosaic parenchymal attenuation (MPA) 36 (72 %), irregular and dilated major airways 33 (66 %) bronchial wall thickening (BWT) 45 (90 %), and interlobular septal wall thickening (SWT) 13 (26 %)” (Ghanei et al. 2004b).
Since about 25 % of the random population had lung air trapping, the presence of more than 25 % of air trapping in a section of lung was considered as diagnostic criterion of BO in this study. The characteristics for HRCT positive slides were studied based on the type and number of lesions in all pulmonary lobes of all 50 patients. Afterwards, the numbers of each type of lesions were counted in the engaged lobes. Air trapping and abnormal pattern were evident in 44 % of patients (Mostafa Ghanei 2011; Ghanei et al. 2011b).
Exhaled HRCT is one of the diagnostic tests that should be performed in the patients who may have small airways involvement, because multiple symptoms of the involvement of small airways, such as air trapping, can be diagnosed only during the exhalation phase. Mosaic parenchyma attenuation is one of the findings that can be diagnosed easily during exhalation. These two signs are the most prevalent abnormal signs during the exhalation state (Bakhtavar et al. 2008). There are some sample HRCT cuts for example in Fig. 7.5a–d.
Fig. 7.5
(a–d) HRCT of SM exposed patients after more than 20 years; emphysema, septal thickening, air trapping are seen (Author captured)
7.10.2 Respiratory Function
7.10.2.1 Polysomnography
In a study that was conducted on 30 SM victims, the relationship between disease intensity and sleep pattern was evaluated based on the GOLD (Global initiative for chronic Obstructive Lung Disease) criteria and polysomnography. Results of this research indicated that patients with a lower intensity of pulmonary symptoms had more hypopnea and more frequent episodes of rapid eye movement. The first stage of sleep in the patients who had higher FEV1 and the fourth stage of sleep in the patients who had higher Diffusing capacity for carbon monoxide (DLCO) was the dominant stages of sleep (Vahedi et al. 2012). These findings can indicate a greater symptomatic response of these patients in more intensive stages of pulmonary disease and asthma.
In chemical victims, in acute phase, “Arterial blood oxygenation (PaO2) and saturation levels were significantly decreased at 12 h. Arterial blood carbon dioxide (PaCO2) significantly increased, and arterial blood pH and bicarbonate (HCO3 −) significantly decreased at 12 h. Shunt fraction was significantly increased at 12 h” (Jugg et al. 2013). Moreover, in chronic phase, there are evidence of imbalance in po2, pco2 and other blood gas parameter (Balali-Mood et al. 2011).
7.10.2.2 Spirometry
Pulmonary Function Tests in Clinical Contact with SM
Pulmonary function tests (PFT) studies are useful for four indices of pulmonary functions: airflow (spirometry), pulmonary volumes, gas exchange (diffusion coefficient) and lung mechanics. In a study which was conducted on 77 persons who attended the SM contaminated areas for at least 1 week, during which they did not have any symptom of SM exposure, it was shown that, although these individuals did not had any initial clinical symptom of the acute phase, they have now late SM toxic effects. Specifically, the PFT pattern was restrictive in 5 % of these patients, obstructive in 5 %, restrictive and obstructive in 8.82 % and normal in 85.3 % (Ghanei et al. 2004a).
Pulmonary Function Tests
In study of the pulmonary function, the chemical victims exposed to SM in acute phase, who did not use suitable protective tools at the time of exposure to the chemical agent, showed an obstructive pattern (53 %), while a restrictive pattern was evident in only 1.5 %, a mixed pattern in 18.7 % and a normal pattern in 21.8 %, based on PFT findings (Sohrabpour 1987).
In another study, which was published in 1997, the pulmonary function was studied in 130 SM victims hospitalized in Isfahan hospitals with acute injury. Of these patients, 11.5 % had restrictive lesions, 32.3 % of them had obstructive lesions, 21.5 % had FEV1 and forced mid-expiratory flow (FMF) reduction (obstruction of small and large ducts) and 10.7 % had only reduction of maximum mid-expiratory flow (MMEF) (small and peripheral respiratory duct obstruction). Only 14 % of the patients had obstructive and restrictive lesion altogether, while 41 % of these people had normal spirometry. Considering the above results, it can be concluded that the most prevalent finding of the abnormal spirometry in the acute phase after SM exposure, is pulmonary obstructive lesion. Spirometry with normal results also played considerable role. It is necessary to note that two thirds of the patients who were above 41 years showed mixed obstructive and restrictive disorders, indicating that the increase of age enhances the intensity of pulmonary complication (M and AR 1997).
In the results of PFT, 35 chemical victims exposed to SM with intensive pulmonary disease for 6 weeks to 1 year showed an obstructive pattern (55 %), restrictive pattern (24 %), small airways involvement (13 %) and normal pattern (6 %) (Sohrabpour et al. 1988).
The most prevalent spirometric changes and clinical symptoms of the flow-volume loop among the people exposed to chemical bombing with mustard included change in the flow-volume loop and smoothness of the middle part of the loop in 18 people (30 %). The obstructions with moderate and mild intensity or changes of flow-volume loop manifested earlier than the spirometric evidence, or these changes were only limited to the flow-volume loop. The maximum changes of the flow-volume loop occurred in the fourth month after injury and the maximum changes in spirometry occurred in the fourteenth month after injury. It was also reported that a distance to the chemical bombing place of up to 500 m did not affect induction and incidence of complication in this group. Nevertheless, it affected the intensity of the complication (Ansarin and Rezvanyeh 1987).
At the end, it was concluded that all obstructive disorders evidenced on the flow-volume loop included lower airways obstruction and no important flow limitation related to upper airway obstruction was found until the end of the 2-year study.
In a cross-sectional study, long-term complications of pulmonary function were studied in 197 chemical victims after 10 years. Findings of these victims were compared with 86 soldiers who were not injured with mustard as control group. In this study, patients were divided into three groups of asthmatic, chronic bronchitis and pulmonary fibrosis patients. Results of PFT were evaluated in all three groups. In this study, the relationship between fibrosis degree and DLCO and PFT test was studied in patients with idiopathic pulmonary fibrosis (IPF), the results revealing that there is only a direct relationship between the intensity of fibrosis and the percentage of DLCO (Emad and Rezaian 1999).
Since the following complementary studies rejected PF and ILD, therefore, the results of the mentioned study cannot be used. Results of a report on 43 patients exposed to SM, among whom the interval between time of injury and their study time was 4–7 years and who had long-term symptoms of injury with SM, showed that RFT had and obstructive pattern in 53 %, 43 % had a restrictive pattern and 5 % had normal pattern. In fact, the most common pattern of the PFT of these patients was obstructive. On the other hand, many of these patients had abnormal clinical and spirometry findings, despite CXR normality. Considering that the patients who were studied at shorter term after injury had a less abnormal pattern, it can be concluded that the progression of pulmonary injury in these patients may be preventable over time (Emad and Rezaian 1999; Attaran et al. 2006).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


