Problem 16 Lower abdominal pain in a 77-year-old woman
A 77-year-old woman presents to the emergency department with acute abdominal pain. She had been feeling unwell over the previous 2 days with left iliac fossa discomfort and constipation. This morning she woke from sleep with worsening acute lower abdominal pain, mainly on the left lower side of her abdomen, constant in nature and aggravated by movement. The pain was associated with some nausea and vomiting. There had been no bowel action for 3 days. There was no rectal bleeding.
Investigation 16.1 Summary of results
| pH | 7.2 (7.38–7.43) |
| pCO2 | 36 mmHg (35–45) |
| HCO3 | 16 (20–24) |
| Lactate | 1.42 (0.50–2.00) |
| Base excess | −9.3 (−3.3–1.2) |
| K | 3.5 (3.8–5.0) |
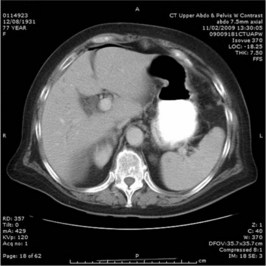
A CT scan of the abdomen is performed. Two representative films are shown in Figures 16.1 and 16.2.
Answers
• Resuscitation: insert an intravenous cannula and rehydrate with colloid solution or isotonic saline (e.g. 250–500 mL of a colloidal solution immediately, then 1 litre of isotonic saline over 1–2 hours). Fluids are essential to support the circulatory system prior to addressing the source of her problem. An indwelling urinary catheter should be inserted to measure urine output and adjust fluids accordingly. An arterial line and a central venous line maybe necessary if patient fails to respond or there is evidence of associated cardiac failure. A nasogastric tube may ease the nausea and vomiting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree