Risk may include torsades de pointes, development of heart failure, unwanted effects on heart rate, and organ damage or dysfunction.
 Benefits may include the potential for improved quality of life and improved long-term outcomes.
Benefits may include the potential for improved quality of life and improved long-term outcomes.
PATHOPHYSIOLOGY
With use of chronic antiarrhythmic medications, consider the following:
• Unique patient characteristics (presence of myocardial ischemia, heart failure, LVH, congenital long QT, etc).
• Drug interactions, known or theoretical.
• Electrolytes, specifically potassium and magnesium.
• Renal function.
• Adverse reactions including toxicities or intolerances.
• Risk of proarrhythmias (prolonged QT, TdP, bradycardia, heart block, wide complex tachycardia, etc).
MANAGEMENT/FOLLOW-UP AND LONG-TERM COMPLICATIONS
Clinical Considerations for Management
• Each class of drugs should be monitored according to the prescribing information.
• Patient encounter for monitoring should always include:
 Patient report of arrhythmia symptoms
Patient report of arrhythmia symptoms
 Medication adherence screening
Medication adherence screening
 Drug interaction assessment and education
Drug interaction assessment and education
 Adverse drug reaction screening
Adverse drug reaction screening
 Completion of objective testing
Completion of objective testing
 Consideration of strategy for rate control and stroke prophylaxis as indicated
Consideration of strategy for rate control and stroke prophylaxis as indicated
 Verbal and written patient education
Verbal and written patient education
• Defining protocols to guide monitoring allows for improved compliance with adhering to requirements.
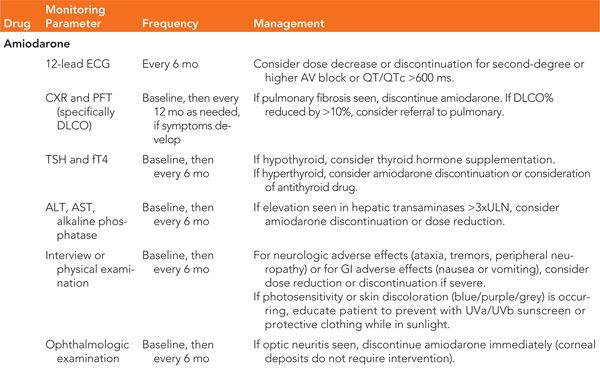
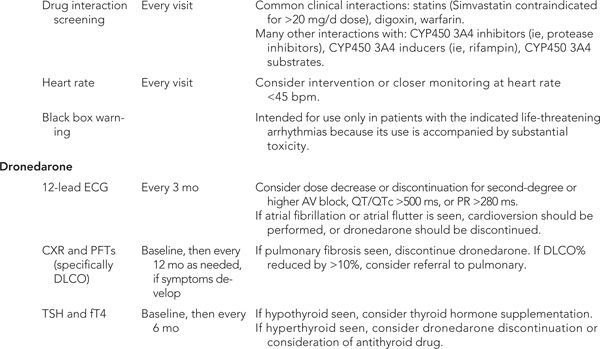
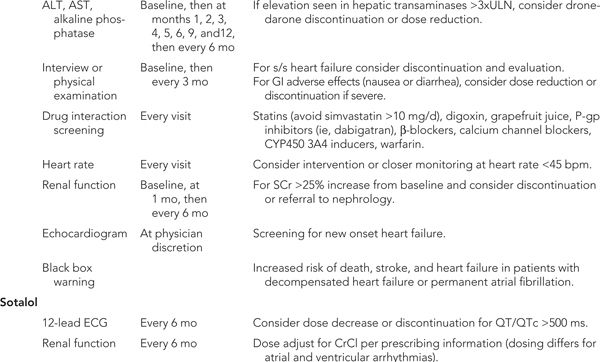
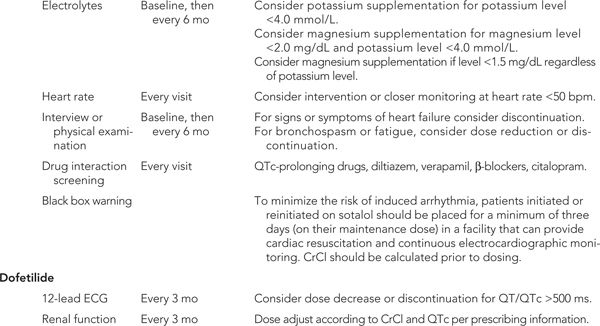
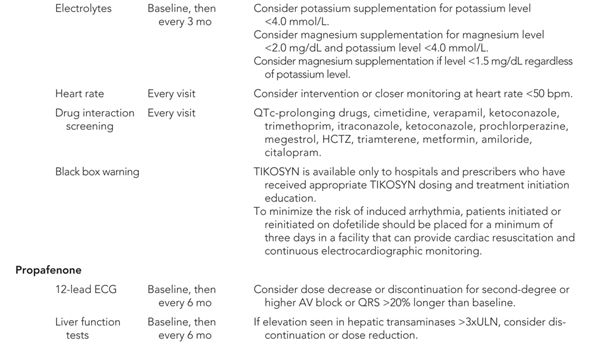
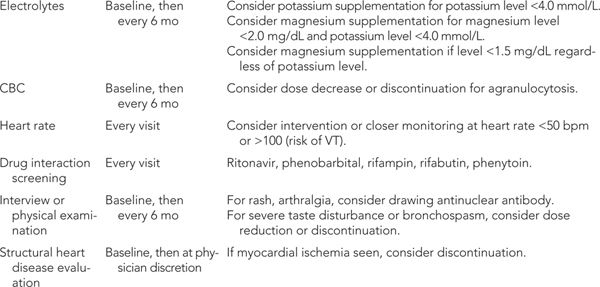
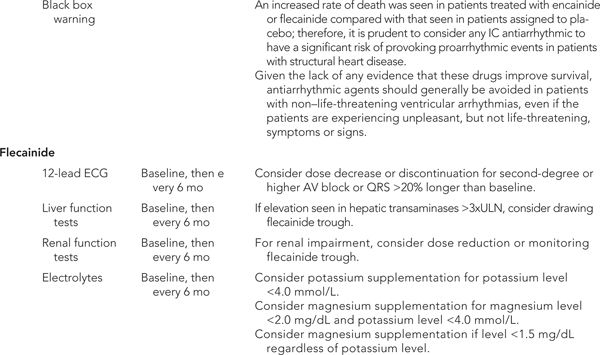
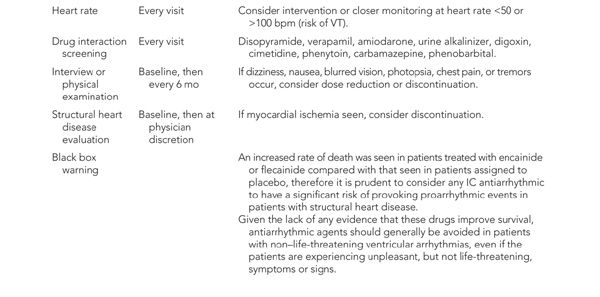
 Example protocols attached (Tables 33-1 and 33-2).
Example protocols attached (Tables 33-1 and 33-2).
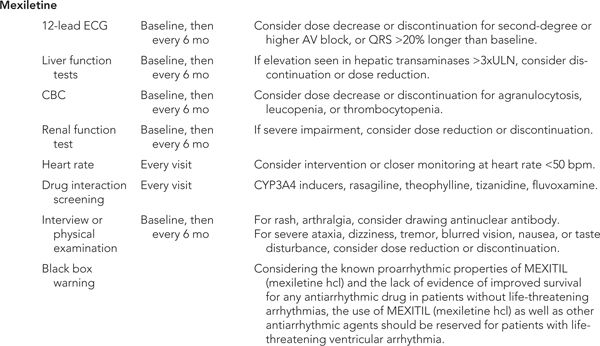
TABLE 33-1 Example Clinical Protocols for Monitoring Long-Term Antiarrhythmic Therapy3,4,5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


