6 Liver disease
Investigations
Routine serum liver biochemical tests
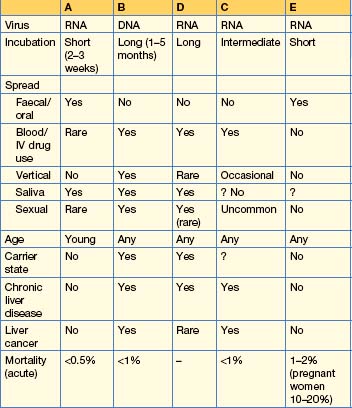
Box 6.1 shows an interpretation of abnormal liver biochemistry.
Box 6.1 Abnormal liver biochemistry — how to proceed
Always check the history and examine the patient for signs of liver disease.
The role of imaging
US is useful for the detection of gallstones and for evaluation of hepatosplenomegaly and other abdominal masses. In focal liver disease, lesions > 1 cm can be detected and US is used to screen patients for hepatocellular carcinoma. Colour flow Doppler will show the direction of blood flow in the portal and hepatic veins. In endoscopic ultrasound, a small, high-frequency US probe mounted on the tip of the endoscope can accurately stage pancreatic tumours (particularly neuroendocrine) and also chronic pancreatitis.
Liver pathology
Jaundice
Jaundice (Fig. 6.1) is due to intra- or extrahepatic cholestasis.
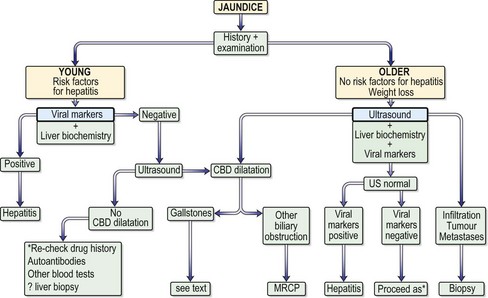
Fig. 6.1 Approach to the patient with jaundice. CBD, common bile duct; MRCP, magnetic resonance cholangiopancreatography; US, ultrasound.
Approach to the patient
Viral hepatitis
Hepatitis A
Management
Hepatitis B
HBV spread also occurs by the IV route (e.g. by transfusion of infected blood or blood products, or by contaminated needles used by drug users, tattooists or acupuncturists) or by close personal contact, such as during sexual intercourse, particularly in men having sex with men (25% of cases in the USA). The virus can be found in semen and saliva.
Clinical features
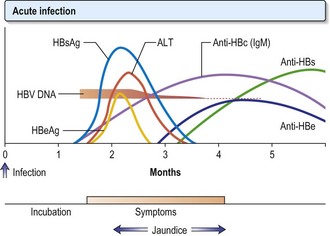
Viral markers
Treatment
HBV infection is mainly asymptomatic and the majority recover completely. Patients should have their HBV markers monitored. If HBcAg is persistent beyond 12 weeks, refer to experts, who may treat patients with nucleoside analogues. Around 1% of patients with acute hepatitis develop fulminant hepatitis (p. 187).
The aim of treatment is the seroconversion of HbeAg (when present), i.e. the development of anti-HBe and the reduction of HBV DNA to undetectable levels by PCR. In addition, normalization of the serum ALT level and histological improvement in inflammation and fibrosis reflects a good response.
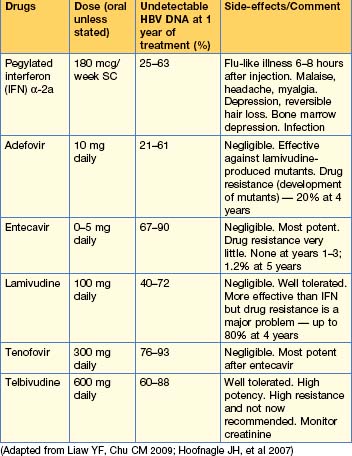
Antiviral agents (Table 6.2)
Choice and duration of treatment
The duration of all treatment, and which combination of antivirals is optimal, are still being assessed. In general, current treatment for HbeAg-positive disease is with pegylated interferon or tenofovir or entecavir. Interferon should be given for 1 year. HbeAg-negative disease requires long-term (many years of) oral therapy. Older patients respond poorly to interferon and should be treated with nucleoside and nucleotide analogues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree