5 Liver and Biliary Tract Disorders
Abnormal liver biochemistry
‘Liver function tests’ are routinely requested.
The doctor asks: would an ultrasound be helpful?
No. This is not the pattern of biliary or pancreatic disease.
On examination you notice a few spider naevi. The liver is not palpable.
The results of the tests performed by the doctor are now available (Table 5.1). HCV antibodies indicate HCV infection (chronic hepatitis) and the patient will require HCV RNA, liver biopsy and possible treatment with anti-viral therapy with pegylated interferon and ribavirin, or with one of the newer protease inhibitors (boceprevir or telaprevir).
Table 5.1 Further investigations into the cause of the abnormal liver function test
| Test | Result | Implication |
|---|---|---|
| Repeat LFTs | Similar to above | |
| Hepatitis A | IgG positive IgM negative | Patient has been infected with HAV in the past or immunised. This virus does not cause chronic liver disease |
| HBsAg | Negative | See below |
| HCV antibodies | Positive | |
| Autoantibody screen | Negative | Positive titres usually found in autoimmune hepatitis |
| Serum ferritin | 110 µg/L | This excludes hereditary haemochromatosis |
Although this patient did not have HBV, you need to know the significance of HBV markers (Table 5.2).
Table 5.2 Significance of viral markers in hepatitis B
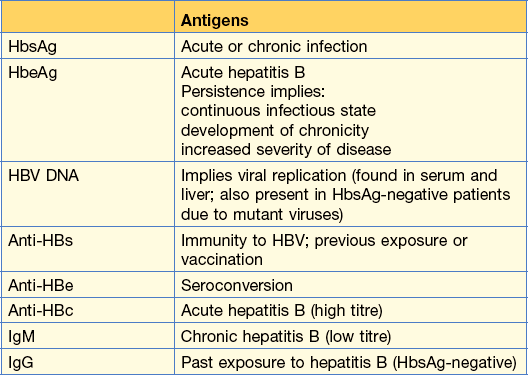
From Kumar and Clark Clinical Medicine, 8th edn, 2012.
Jaundice
Jaundice is detected clinically when the serum bilirubin is greater than 50 µmol/L (3 mg/dL).
Case history (1)
Abdominal examination is unhelpful; there were no signs of chronic liver disease.
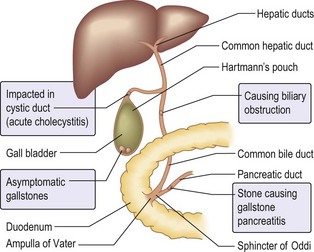
The blood tests showed a raised serum bilirubin, an ALT of 50 units and a high alkaline phosphate of 410 units. You order an ultrasound examination of the liver and biliary tree as you suspect that she has got gallstone disease (Fig. 5.1).
Ultrasound in extra-hepatic obstruction can show:
• Dilatation of the intra-hepatic biliary tree
• Dilatation of the common bile duct
• Gallstones in the gall bladder
• Gallstones in the biliary tree
In this patient, the ultrasound showed gallstones in the gall bladder and a dilated common bile duct. Provided this patient’s clotting is satisfactory, the next procedure should be an ERCP. This would enable a better visualisation of the system and would allow a gallstone that is causing the obstruction in the common bile duct to be removed. A sphincterotomy would need to be performed beforehand and the stone could be removed with a basket or a balloon. If the stone is very large, the stone can be crushed and the debris removed. In an elderly patient, stent insertion to maintain drainage is an option.