Leiomyosarcoma
Elizabeth A. Montgomery, MD
Key Facts
Terminology
Malignant neoplasm composed of cells exhibiting smooth muscle differentiation
Etiology/Pathogenesis
Epstein-Barr virus associated in immunosuppressed patients
Clinical Issues
Superficial or deep soft tissue mass, often asymptomatic, in extremities
Retroperitoneum most common site
Retroperitoneal and inferior vena cava lesions more common in women
Uncommon: 10-15% of extremity sarcomas
Most common sarcoma type if uterine examples are included
Treatment is complete surgical excision
Prognosis is site and stage dependent, as with other sarcoma types
Microscopic Pathology
Perpendicularly oriented fascicles of spindle cells
Brightly eosinophilic cytoplasm
Blunt-ended nuclei
Nuclear atypia
Ancillary Tests
Labels as per smooth muscle: Desmin, actin, calponin, caldesmon
Some cases label with keratins
Top Differential Diagnoses
Sarcomatoid squamous cell carcinoma
Atypical fibroxanthoma (AFX)
TERMINOLOGY
Abbreviations
Leiomyosarcoma (LMS)
Definitions
Malignant neoplasm composed of cells exhibiting smooth muscle differentiation
ETIOLOGY/PATHOGENESIS
Infectious Agents
Epstein-Barr virus (EBV) associated in immunosuppressed patients
Occasional examples are radiation associated
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon: 10-15% of extremity sarcomas
Most common overall sarcoma type if uterine and visceral examples are included
Age
Middle-aged adults
Gender
No gender preference overall
Presentation
Cutaneous LMS presents as a single nodule or plaque-like tumor
May be ulcerated or show serum crusting/hemorrhage
Deep soft tissue tumors present as a mass, often asymptomatic, in extremities
Retroperitoneum most common site
Vena cava examples often symptomatic
Uterine examples considered separately with unique diagnostic criteria
Treatment
Surgical excision
Radiation
Chemotherapy for metastatic tumors
Prognosis
Outcome site and stage dependent as with other sarcoma types
Lesions restricted to cutis essentially never metastasize
Some observers have advocated diagnosing them as “atypical smooth muscle tumors”
Subcutaneous lesions
Up to 1/3 of tumors metastasize
10-20% of patients with subcutaneous lesion die of disease
Retroperitoneum: About 80% of patients die of disease, typically with metastases
Bone: Metastases in up to 1/2 of patients
Vena cava: 5- and 10-year survival 50% and 30%, respectively
Head and neck: Over 1/2 metastasize
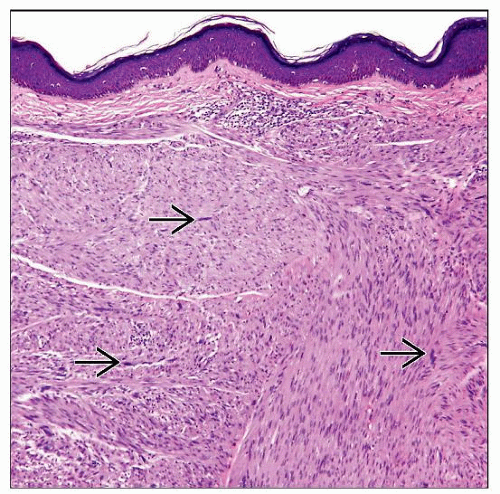
MICROSCOPIC PATHOLOGY
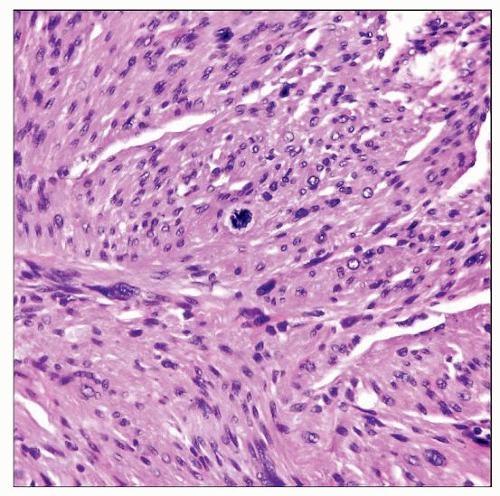
Histologic Features
Perpendicularly oriented fascicles of spindle cells
Cells show brightly eosinophilic cytoplasm
Blunt-ended nuclei with nuclear atypia
Some examples are epithelioid-appearing
Any number of mitoses sufficient in subcutis, scrotal lesions, or deep soft tissue if nuclear atypia is present
In vulva, some observers offered > 5 mitosis per 10 HPF as “cutoff,” but recurrences reported in lesions with any mitotic activity
Predominant Pattern/Injury Type
Fascicular
Predominant Cell/Compartment Type
Mesenchymal, smooth muscle
Variant and Special Forms
Epithelioid leiomyosarcoma
Literature confounded because many epithelioid gastrointestinal stromal tumors (GIST) were termed epithelioid LMS in past
Found anywhere in body
Distinct epithelioid morphology, but more nuclear atypia than GISTs
Older studies reported smooth muscle actin (SMA) and muscle specific actin (MSA) positive, desmin negative immunophenotype, but desmin labels most lesions using modern methods
Possible reflection of misdiagnosed GISTs
Less sensitive desmin antibodies in past
Myxoid leiomyosarcoma
Grossly gelatinous
Extensive myxoid change, but zones of typical leiomyosarcoma allow diagnosis
Express desmin and actin
Subset labels with keratin antibodies
Tend to be low grade
Clinicopathologic features otherwise same as typical leiomyosarcoma
Inflammatory leiomyosarcoma
Characterized by dense inflammation that masks underlying lesion
Histiocytes, xanthoma cells, lymphocytes, neutrophils
Areas of more typical morphology must be sought
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree