Chapter 37 Leg Swelling (Case 23)
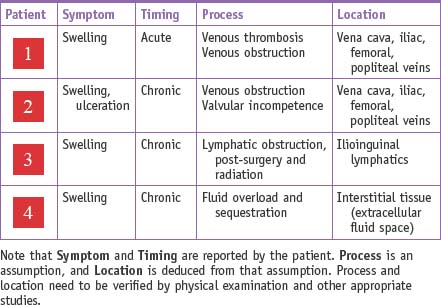
| Patient 1 | 33-year-old woman with a 2-day hx of left calf pain and swelling |
| Patient 2 | 54-year-old man with a 3-year hx of right leg swelling and medial calf ulcer |
| Patient 3 | 55-year-old man with left leg swelling 2 years following prostatectomy, pelvic lymph node dissection, and adjuvant pelvic radiation |
| Patient 4 | 66-year-old man with bilateral leg swelling and shortness of breath |
In each chapter in this section the Differential Diagnosis box has been replaced by a Framework for Clinical Thinking box to help direct the sorting process. See the editor’s note on page 249.
PATIENT CARE
History
• Patients should be asked to describe the acuity of onset and the character of any associated pain. Is the swelling unilateral or bilateral? Were there any antecedent events that predated the leg swelling? Patients with chronic venous insufficiency usually have an antecedent event predating the onset of their symptoms: ask about a hx of DVT, long bone fracture, prior surgery. or prolonged immobilization.
• Pain experienced by a patient with leg swelling can have specific qualities based on the underlying pathology: DVT—a dull ache aggravated by ambulation and improved with elevation; superficial thrombophlebitis—localized pain overlying the area of thrombosis; lymphedema, in general, is painless unless associated with a superimposed cellulitis.
Physical Examination
• The examination begins with observation. In patients with venous obstruction, the location of the swelling will often indicate the level of obstruction. Calf and leg swelling generally indicate an occlusive process involving the femoral or popliteal veins. Swelling of the entire extremity, including the thigh, suggests an iliofemoral obstructive process.
• It is important to objectively quantify the extent of swelling, which can be done by measuring the diameter of the leg below the tibial tuberosity and above the malleoli.
• The type of edema should be documented. Venous disorders will produce pitting edema whereas the swelling associated with lymphedema is nonpitting. Toe and foot swelling is almost exclusively found in patients with lymphedema.
• Skin changes should be noted. Chronic venous skin changes are generally associated with deep venous incompetence and include lipodermatosclerosis and ulceration in proximity to the medial malleolus. Superficial venous insufficiency usually results in serpiginous varicosities involving the thigh, calf, and ankle with a distribution related to the origin of the reflux.
• Ulceration is a common late finding of deep venous insufficiency. Rarely will the patient have venous ulceration from isolated superficial venous insufficiency; however, it is common for both deep and superficial venous insufficiency to coexist.
• Assessment of the pulse status is critical, as many patients will have coexisting arterial occlusive disease. As it may be difficult to palpate pulses because of the swelling, a Doppler examination should be used to confirm the presence and character of the flow. If there is any question about arterial inflow, ankle-brachial indices should be obtained.
| Clinical Entities | Medical Knowledge |
|---|---|
| Acute Deep Venous Thrombosis | |
| PΦ | Acute thrombotic obstruction of the deep veins of the lower extremity results in venous stasis/pooling and elevated venous pressures distal to the obstruction. Typical patterns are iliofemoral, involving the iliac and femoral veins, and femoropopliteal venous thrombosis. |
| TP | The typical patient (Patient 1) presents with lower extremity swelling, primarily in the calf, which increases with ambulation and improves with rest and elevation. The patient will often report an antecedent event or predisposing condition such as recent surgery, trauma, travel, prolonged immobilization, or a dx of cancer. On physical examination, the circumference of the extremity will be significantly increased (>2cm) compared with the uninvolved extremity. |
| Dx | The acute onset of leg swelling with evidence of acutely obstructing deep venous thrombus (DVT) on lower extremity venous duplex imaging is diagnostic. |
| Tx | Therapy consists of therapeutic anticoagulation with heparin and Coumadin. Local symptoms are controlled by elevation of the extremity. The leg is wrapped with compression bandages and the patient is allowed to ambulate. With the control of acute swelling, compression bandages can be replaced with graduated compression stockings. If the patient has iliofemoral venous thrombosis, thrombolytic therapy may be an option in the patient without a prior hx of DVT and the recent (within 7 days) acute onset of symptoms. See Sabiston 68, Becker 36. |
Superficial Thrombophlebitis (Acute Superficial Venous Occlusion)
| PΦ | Thrombosis of the superficial veins results in localized inflammation surrounding the affected veins. As opposed to deep venous obstruction, venous hemodynamics in the lower extremity are not usually affected. |
| TP | The patient typically presents with a painful, erythematous, area of induration involving the medial aspect of the thigh or calf. The patient will usually have associated varicosities that may also be involved. No specific position or activity makes the pain better or worse. Ambulation is usually not significantly affected. |
| Dx | The dx is made by identifying a palpable cord in proximity to the area of induration and erythema. The dx is confirmed by documenting occlusion of a superficial vein or varicosity using lower extremity venous duplex imaging. |
| Tx | The tx of superficial thrombophlebitis consists of nonsteroidal anti-inflammatory agents, rest, elevation of the affected extremity and warm moist compresses over the affected area. See Sabiston 68, Becker 36. |
Chronic Deep Venous Insufficiency
| PΦ | Chronic venous insufficiency (venous stasis ulceration, post-phlebitic syndrome) is frequently a result of the venous valvular dysfunction that follows DVT. Because symptoms develop 5 to 10 years after an episode of DVT, the patient may not recall the initial event. As a result, the patient should also be questioned about a prior hx of predisposing risk factors, such as long bone fracture, pelvic surgery or prolonged immobilization. Symptoms progress from mild swelling to induration and lipodermatosclerosis (a brownish discoloration and induration due to fibrosis of the subcutaneous tissues and hemosiderin deposition), and ultimately to ulceration. Ulceration is most common over the medial leg. |
| TP | In patients with chronic deep venous insufficiency, there can be significant swelling and edema. Lipodermatosclerosis and ulceration may be present at the level of the medial malleolus (Patient 2). Patients complain of pain and heaviness, generally worse at the end of day, with associated swelling. |
| Dx | The dx of deep venous insufficiency and venous reflux is confirmed with lower extremity venous duplex imaging. In a significant number of patients where symptoms are mild to moderate, venous reflux may not be documented on duplex examination, but may be assumed. If necessary, venography may be used to confirm the dx, but generally the findings will not alter the therapy. |
| Tx | Tx of chronic venous insufficiency consists of conservative measures, including the use of elevation and graduated compression stockings. If ulcerations are present, medicated compression wraps (Unna’s boot) are usually employed. The results of surgical repair, attempting to restore valve function, have generally been dismal. See Sabiston 68, Becker 35. |
Superficial Venous Insufficiency (Varicose Veins)
| PΦ | Superficial venous insufficiency is due to incompetent valves at the saphenofemoral junction and within the greater saphenous vein. This condition may be hereditary and frequently follows childbirth. The valve dysfunction results in an enlarged saphenous vein with the development of subcutaneous varicosities, spider veins, and telangectasias. |
| TP | The patient will complain of varicosities associated with pain, heaviness, and an aching sensation involving the leg. Swelling is usually minimal, but if present is worse at the end of the day. Elevation of the legs generally provides symptomatic relief. |
| Dx | Lower extremity venous duplex imaging can also be used to confirm saphenous or perforator vein incompetence. Clinically, the Trendelenberg test can be used to identify saphenous-dependent varicosities. Prompt refilling of the varicosities on standing suggests the presence of incompetent perforating veins. |
| Tx | Tx of superficial venous (saphenous or perforating vein) reflux and varicosities is based on the elimination of valvular incompetence and venous reflux. Tx options include saphenous vein stripping or endovenous ablation, perforation ligation, and stab phlebectomy. See Sabiston 68, Becker 35. |
| PΦ | Primary lymphedema results from an intrinsic abnormality of the lymphatic system. It is classified relative to the age at onset. Congenital lymphedema presents at birth and is more common in males. Lymphedema praecox is the most common form and presents at the onset of puberty. Lymphedema tarda generally presents in patients over 35 years of age. Lymphedema praecox and lymphedema tarda affect women more commonly. |
| TP | The clinical presentation is usually associated with painless leg swelling or mild discomfort. The presentation is usually unilateral, and elevation of the extremity generally does not result in resolution of the edema. As the disease progresses, the extremity develops a spongy, firm consistency. Ulcerations are rare, although recurrent episodes of cellulitis can occur. |
| Dx | Dx is usually based on hx and physical examination. Lower extremity venous duplex imaging is obtained to rule out any deep venous abnormalities. Lymphoscintigraphy is obtained when there is a question regarding the etiology of the swelling. |
| Tx | Tx of primary lymphedema is usually directed at conservative measures, including prevention of skin infection and massage therapy to reduce the interstitial fluid component. Aggressive tx of infections in these patients is necessary, and often a prescription (antibiotic coverage for gram-positive organism) is given to the patient to take at the first sign of infection. This is to prevent scarring of the lymphatics related to infection. Compression therapy is the mainstay of tx, which is usually instituted after the patient has undergone manual lymph drainage in the form of either physical therapy massage or mechanical compressive therapy. See Sabiston 69, Becker 35. |
| PΦ | Secondary lymphedema is most commonly seen in foreign countries, or following foreign travel, and is primarily caused by infection (filariasis). The most common causes in the United States result from injury to, or removal of, regional lymph nodes (Patient 3). Specific causes of secondary lymphedema include cancer (tumor, surgery, or radiation), infection, inflammation, or trauma. |
| TP | The patient presents with swelling and heaviness of the affected limb. Often the patient will present with erythema and cellulitis superimposed on the lymphedema. |
| Dx | The dx of secondary lymphedema is usually made by hx and physical examination, combined with a prior hx of trauma or infection involving the lymphatics. Lymphoscintigraphy is reserved for those cases where the dx is in question. |
| Tx | The tx of secondary lymphedema is nonsurgical with the focus on controlling swelling and the incidence of cellulitis. Patients who have infections and cellulitis should be treated aggressively with antibiotics. See Sabiston 69, Becker 35. |
Systemic Causes: Congestive Heart Failure, Liver Failure, Renal Failure
| PΦ | The common theme among systemic causes of lower extremity swelling is fluid overload or fluid retention. The most common cause of bilateral lower extremity swelling is cardiac dysfunction and congestive heart failure (CHF) (Patient 4). Often the first manifestation of CHF is progressive swelling of the legs. The swelling associated with CHF, unlike that seen with venous disorders, is generally not affected by leg elevation and is present upon awakening in the morning. It may also be associated with dyspnea and orthopnea. |
| TP | The typical patient may have preexisting disease, although peripheral edema can be the initial presentation of CHF, liver failure, or chronic renal insufficiency. It may also be seen in poorly compliant patients, with a hx of preexisting disease. |
| Dx | Dx is clinical and can be based on echocardiography or laboratory studies. |
| Tx | While support stockings can be helpful in controlling lower extremity swelling, tx should be focused on the underlying etiology. See Sabiston 69, Becker 35. |
a. May-Thurner syndrome: May-Thurner syndrome is related to stenosis or obstruction of the left common iliac vein as it crosses under the right common iliac artery. It is seen in young female patients, especially around the time of childbirth when the uterus compresses the left common iliac vein. Patients generally present with unilateral swelling of the left lower extremity that is aggravated by exercise and activity. It is generally worse at the end of the day. Dx can be confirmed by venography, CTV, or MRV. Tx consists of angioplasty and stenting of the obstructed segment of the vein.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree