Left Hepatic Trisectionectomy
Jason A. Castellanos
Kamran Idrees
DEFINITION
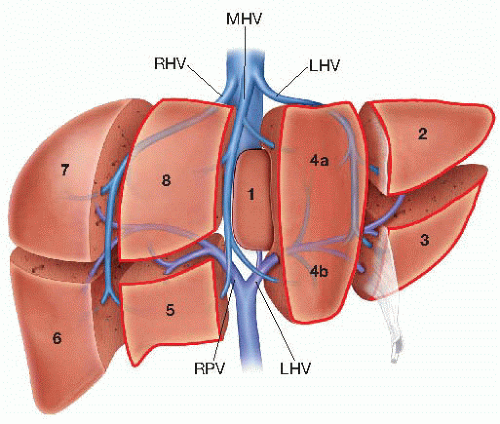
First described by Starzl et al.1 in 1982, this procedure entails a standard left hepatic hepatectomy (segments 2, 3, and 4) as well as resection of the right anterior sector (segments 5 and 8) (FIG 1).
This operation is performed in a patient with a primary hepatic tumor or metastases involving the left liver invading across the middle hepatic vein toward the right hemiliver and/or portions of segments 5 and 8. Additionally, patients with hilar cholangiocarcinoma may require this procedure in order to obtain tumor-free margins.
PATIENT HISTORY AND PHYSICAL FINDINGS
Careful evaluation of the patient is required to ensure that the future liver remnant provides adequate liver function after resection. This should include assessment of liver function and exclusion of cirrhosis in addition to volumetric evaluation of the expected remnant liver volume on crosssectional imaging.
It is imperative to rule out portal hypertension or chronic liver disease, as a majority of the liver will be resected during this procedure.
Details regarding prior therapy should be obtained.
IMAGING AND OTHER DIAGNOSTIC STUDIES
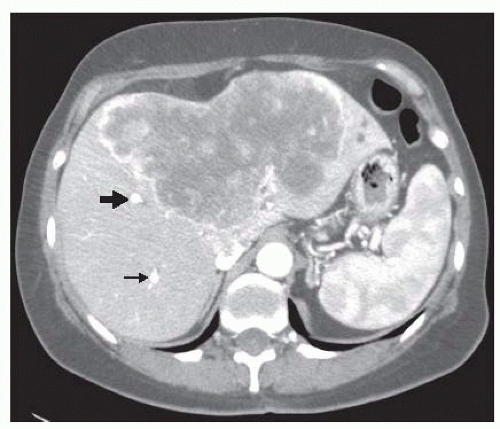
Obtain either a liver-devoted magnetic resonance imaging (MRI) or contrast-enhanced, triphasic computerized tomography (CT) scan of the abdomen to identify tumor/s and its relationship to hilar structures and hepatic veins, anatomic variations of hilar vasculature, and assess for radiographic signs of cirrhosis (FIG 2).
Identify tumor and assess margins for possibility of R0 resection as well as volumetric assessment of future liver remnant.
For metastatic disease, perform a complete staging evaluation as appropriate for the particular primary neoplasm.
Intraoperative ultrasound is essential to define margins; exclude presence of disease in the planned liver remnant and visualize hepatic inflow and outflow.
SURGICAL MANAGEMENT
Preoperative Planning
Assessment of the future liver remnant volume should be calculated with preoperative imaging to ensure adequate liver function after resection—greater than 20% in patients with normal liver function, greater than 30% for patients with evidence of liver disease (nonalcoholic fatty liver disease, chemotherapy-associated steatohepatitis, etc.), and greater than 40% in cirrhotic patients.2,3 If the remnant liver volume is deemed to be too small, then portal vein embolization may be used as an adjunct therapy to hypertrophy the future liver remnant prior to hepatectomy.
Positioning
The patient should be placed in the supine position with the right arm tucked and prepped from the nipples to the pubis bilaterally.
TECHNIQUES
DIAGNOSTIC LAPAROSCOPY
Our practice is to perform an initial diagnostic laparoscopy to ensure that there is no evidence of peritoneal disease.
A supraumbilical incision is made through the skin and subcutaneous tissue using the Hasson technique and a trocar is introduced into the abdomen, which is then insufflated to a pressure of 15 cm H2O.
The abdomen is explored including the hilum of the liver to assess for metastatic disease and periportal adenopathy. If there are no contraindications to operation, we then proceed to incision.
INCISION
A bilateral subcostal incision is made, with superior extension in the midline to the xiphoid process, and a self-retaining retractor is placed. Another option is a midline incision to just above the umbilicus with a rightward extension (FIG 3).
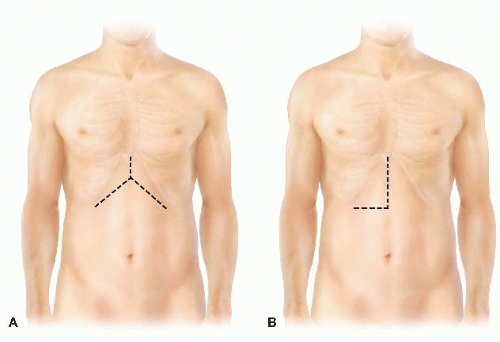
FIG 3 • Incisions for left trisectionectomy include (A) bilateral subcostal incision and (B) long midline incision with rightward extension.
The xiphoid process may be excised in order to enhance exposure of the confluence of the hepatic veins into the suprahepatic inferior vena cava (IVC).
The abdomen is inspected again for evidence of distant metastases that would contraindicate proceeding with operation.
INSPECTION OF THE HILUM, CHOLECYSTECTOMY
The hilar structures are palpated in order to define any anatomic variations (e.g., a posterior pulsation indicates a replaced/accessory right hepatic artery originating from the superior mesenteric artery).
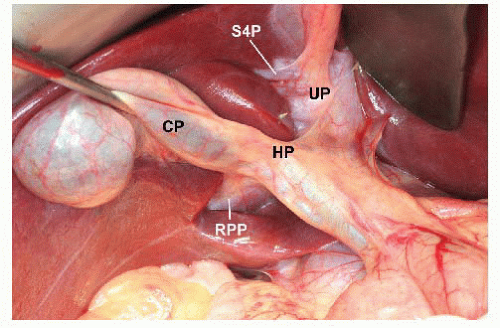
The cystic duct and cystic artery are identified and ligated, and a cholecystectomy is performed (FIG 4).
MOBILIZATION OF THE LIVER
The round ligament is ligated and divided, and the falciform, left triangular and coronary ligaments are divided to the level of the hepatic veins. The right coronary and triangular ligaments are transected, exposing the bare area of the liver.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree