Left Hemicolectomy: Laparoscopic Technique
Erik Askenasy
DEFINITION
A “left hemicolectomy” can be a nebulous term because three colonic segments lie in the left abdomen: the splenic flexure, the descending colon, and the sigmoid colon. At times, this can lead to consternation during surgical planning or even intraoperatively. Remembering that the location of the pathology guides the extent of colonic resection as well as the associated vascular and regional lymph nodes can provide much needed clarity. Additionally, understanding the vascular anatomy of the left colon and its common variations is essential for a well-vascularized and tensionfree anastomosis.
The left colon develops embryologically from the hindgut and contains three segments: the splenic flexure, the descending colon, and the sigmoid colon. The splenic flexure is located in the left upper quadrant and is supplied by antegrade flow from the left branch of the middle colic as well as retrograde flow from the left colic artery. Griffith’s point is typically found in the splenic flexure and refers to the watershed area between these two arteries and represents a circulatory communication between the superior and inferior mesenteric arteries. The descending colon lies in between the sigmoid colon and the splenic flexure and is supplied by the left colic artery. Finally, the sigmoid colon is located in the left lower quadrant and is supplied by the sigmoidal arteries, branches of the inferior mesenteric artery (IMA) after the takeoff of the left colic artery. In this chapter, we will focus on the splenic flexure and the descending colon.
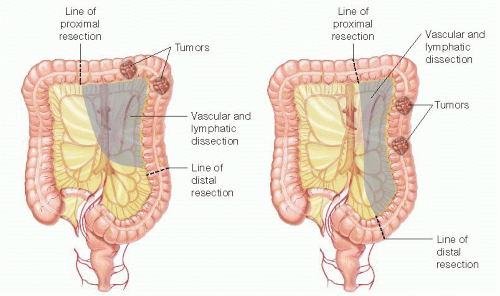
A surgeon must be ready for “surprises” when entering the abdomen for a lesion in the descending colon, because there can be wide variation between the location of the target lesion as reported during flexible colonoscopy and the actual location found during surgery. The exact type and extent of resection will be dictated by the lymphovascular pedicles associated with the location of the target lesion (FIG 1).
Less pain
Faster return to work
Quicker return of bowel function
Shorter hospital stay
DIFFERENTIAL DIAGNOSIS
Common indications for laparoscopic left hemicolectomy
Cancer of the splenic flexure or descending colon
Diverticular disease and its sequelae, including colovesicular or colovaginal fistulas
PATIENT HISTORY AND PHYSICAL FINDINGS
Most patients with early-stage colon cancer are asymptomatic, with lesions found on colonoscopy performed for screening purposes or secondary to a positive fecal occult blood test.
Late-stage colon cancer can present with abdominal pain, unexplained weight loss, melena, iron deficiency anemia, or a change in bowel habits. Obstructive symptoms are typically secondary to circumferential tumors.
Patients with uncomplicated diverticulitis report episodic pain in the left lower quadrant associated with fever, changes in bowel habits, and/or bloating.
The spectrum of symptomatology for complex diverticulitis can be as benign as those for uncomplicated
diverticulitis but can progress to localized or even generalized peritonitis.
Patients with neoplastic or inflammatory erosion into adjacent organs, such as the bladder or vagina, can present with pneumaturia, fecaluria, or fecaloid vaginal discharge.
A thorough family history of colon or rectal cancer, polyps, and/or other malignancies should be elicited.
Physical examination should include the following:
Abdominal examination, focusing on localized tenderness, masses, and previous scars
Digital rectal examination to assess for blood as well as sphincter function
IMAGING AND OTHER DIAGNOSTIC STUDIES
A full colonoscopy is essential. If a lesion is identified and it is suspicious for malignancy, the area should be tattooed to aid in intraoperative localization.
In malignancy, a triple-phase computed tomography (CT) chest/abdomen/pelvis scan is performed to evaluate for metastases and locoregional extent of disease as well as to delineate the vascular anatomy. A preoperative carcinoembryonic antigen level should also be obtained.
In diverticulitis, a routine CT abdomen/pelvis scan with oral and intravenous (IV) contrast is obtained.
SURGICAL MANAGEMENT
Preoperative Preparation
Although preoperative bowel preparation is controversial, we routinely use it, as it makes the bowel easier to handle.
Chlorhexidine shower the evening prior to surgery
Normothermia maintained with Bair Hugger (36°C to 37°C) perioperatively
Euglycemia maintained perioperatively
One gram of Rocephin and 500 mg of Flagyl are administered within 1 hour of skin incision.
Hair clippers are used to clear the field.
Chlorhexidine is used for skin preparation; Betadine is used for perineal preparation.
Preoperative time-out and briefing
Equipment and Instrumentation
One Hasson trochar, one 12-mm port, and two 5-mm ports
A 10-mm, 45-degree camera (may use 5 mm if quality of camera is acceptable)
Atraumatic bowel gaspers, laparoscopic endoscissors, and a 5-mm energy device
Patient Positioning and Surgical Team Setup
For pathology proximal to the mid-descending colon, the patient is placed on a supine position. Otherwise, the patient is placed on a lithotomy position.
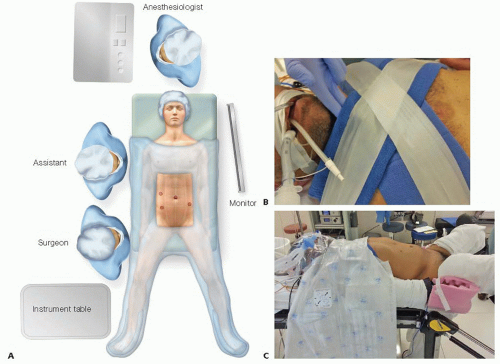
Both arms are tucked and padded. Wide silk tape is applied over two towels across the patient’s chest in an “X” figure to secure the patient (FIG 2B).
The patient is positioned such that the anus is easily accessible.
The legs are placed in Allen stirrups, making sure the heel is flush against the base. Pressure points are padded posteriorly and laterally.
The thighs are positioned parallel with the floor to minimize encroachment on the surgeon’s right operating arm (FIG 2C).
Thighs are wrapped with warm blankets to minimize heat loss during surgery.
Draping is performed to allow for easy access to the perineum.
The surgeon starts at the patient’s right lower side with the assistant to his or her left. The assistant drives the camera while the surgeon uses both working ports (FIG 2A).
A single monitor is needed and located on the patient’s left side, across from the surgeon and at or slightly below eye level.
All laparoscopic cables should come in from the patient’s upper left side. All energy devices, Bovie, and suction should come in from the patient’s upper right side. This setup prevents cluttering of the field and facilitates movement of the team around the table.
TECHNIQUES
PORT PLACEMENT AND OPERATIVE FIELD SETUP
A Hasson trochar is placed at the umbilicus. This serves as the camera port as well as the extraction site. If the pathology is located in the distal descending colon, a 12-mm port is placed in the right lower quadrant and a 5-mm port is placed in the right midquadrant. If the pathology is more proximal, then the two right abdominal ports are shifted cephalad a few centimeters (FIG 2A).
A 5-mm port can be placed in the left lower quadrant to aid with takedown of the white line of Toldt and with the splenic flexure mobilization.
OPERATIVE STEPS
Although slight adjustments may be necessary based on the exact location of the lesion, laparoscopic surgery for lesions in the splenic flexure or in the descending colon should be standardized to maximize operative efficiency, following these sequential steps:
Placement of the omentum above the transverse colon
Transection of the superior mesenteric vein (SMV)
Transection of the left colic artery or the IMA (depending on pathology location)
Medial to lateral dissection of the descending mesocolon
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree