Lateral Pancreaticojejunostomy with (Frey) or without (Puestow) Resection of the Pancreatic Head
Kevin E. Behrns
Jose G. Trevino
DEFINITION
Chronic pancreatitis is an inflammatory disease that encompasses a spectrum of morphologic, histologic, and clinical features, which range from subclinical inflammatory changes evident only in histologic specimens to marked morphologic gland destruction accompanied by acinar cell dropout, prominent deposition of fibrous extracellular matrix, and pancreatic duct strictures.
DIFFERENTIAL DIAGNOSIS
Acute pancreatitis
Autoimmune pancreatitis
Pancreatic adenocarcinoma
Intraductal papillary mucinous neoplasm (IPMN)
PATIENT HISTORY AND PHYSICAL FINDINGS
Advanced stages of chronic pancreatitis manifest clinically by disabling pain and pancreatic exocrine and endocrine insufficiency.1,2 The most prominent etiology of chronic pancreatitis is excess consumption of alcohol.
Other forms of chronic pancreatitis including autoimmune pancreatitis, paraduodenal pancreatitis, and familial pancreatitis are attributed to genetic mutations.2, 3, 4, 5
Differentiating alcoholic chronic pancreatitis from autoimmune pancreatitis, especially focal autoimmune pancreatitis,6 and adenocarcinoma of the pancreas may require extensive evaluation and prove challenging.7
Important risk factors that exacerbate the development of chronic pancreatitis include alcohol use and smoking cigarettes.8,9
A detailed history of alcohol consumption should be obtained; heavy alcohol use (>5 drinks per day) is present in the majority of patients with chronic pancreatitis.8,9
The pain associated with chronic pancreatitis may be either episodic or persistent.2 Episodic abdominal pain has a duration of 1 to 2 weeks and is interrupted by pain-free periods of a few months. Persistent pain occurs daily but on occasion may spontaneously resolve for a period of a month or more.10
The weight loss seen in chronic pancreatitis typically occurs over months to years, but it may be more rapid if morphologic changes such as pseudocyst formation induce gastroduodenal obstruction.
Other complications of chronic pancreatitis include jaundice from biliary obstruction and upper gastrointestinal bleeding from gastric varices secondary to splenic vein obstruction.
IMAGING AND OTHER DIAGNOSTIC STUDIES
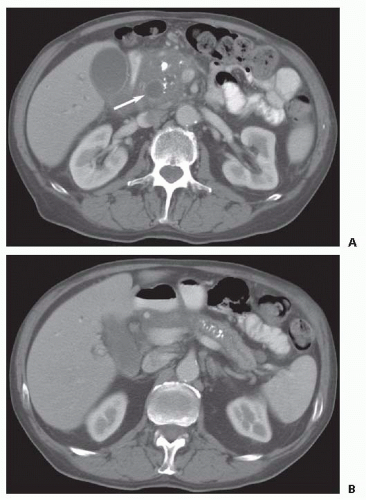
Computed tomography (CT) is the imaging procedure of choice. Intravenous contrast-enhanced, multiplanar, thinslice CT provides excellent imaging of pancreatic parenchymal and ductal anatomy.11 CT characteristics of chronic pancreatitis include an enlarged pancreatic head with multiple calcifications and a dilated pancreatic duct distally (FIG 1).
Detection of early-stage disease may be enhanced by magnetic resonance (MR) with cholangiopancreatography (MRCP) with or without secretin administration. Morphologic changes
in the pancreatic duct and hydrodynamic-significant strictures may be evident on these images.12
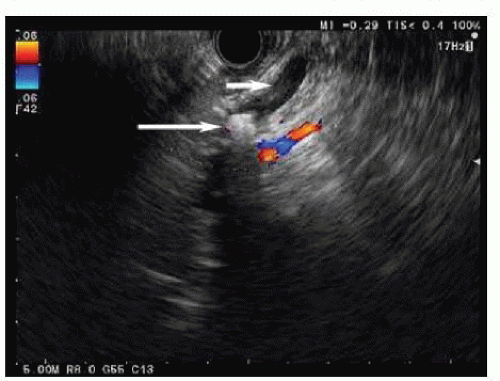
FIG 2 • Endoscopic ultrasound demonstrating a dilated pancreatic duct (short arrow) with a calculus (long arrow) in a patient with chronic pancreatitis.
Endoscopic ultrasound (EUS) with or without functional testing by administration of secretin may aid in the diagnosis of early fibrosis in chronic pancreatitis (FIG 2). EUS has a sensitivity of 84% and a specificity of 100%, correlating with histology for chronic pancreatitis.13 Furthermore, EUS is advantageous when mass lesions are present in chronic pancreatitis because EUS-guided biopsy is the most reliable method of confirming malignancy.
Imaging of the pancreatic duct prior to surgical intervention is essential because all strictures and intraductal calculi must be addressed by the operative approach. Ductal anatomy can be delineated by MRCP or endoscopic retrograde cholangiopancreatography (ERCP). ERCP is often performed in the context of pancreatic duct stenting as endotherapy often precedes operative management.
SURGICAL MANAGEMENT
Operative management of chronic pancreatitis by lateral pancreaticojejunostomy with or without pancreatic head resection is indicated in patients with disabling abdominal pain, weight loss, and evidence of pancreatic duct obstruction.14 Morphologic characteristics are associated with outcomes. An excellent response to pancreatic head resection with pancreaticojejunostomy is most likely in the setting of an enlarged head of the pancreas and a distally dilated pancreatic duct.15
Table 1: Preoperative Checklist for Patients Undergoing a Frey Procedure | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree