Laparoscopic Right Hemicolectomy
Morris E. Franklin
Karla Russek
Introduction
The first laparoscopic-assisted right hemicolectomy was described in 1992 and since then several authors have published their techniques. The indications for laparoscopic right colon surgery have been extended from early colon cancer to advanced cancer because this approach has several distinct advantages in comparison to open surgery, including lesser use of analgesics, earlier return of bowel motility, a shorter hospital stay, faster perioperative recovery, and lower incidence of wound infections and hernia rates. A meta-analysis of the results of 2,512 procedures from 12 randomized clinical trials reported improved short-term outcomes for laparoscopic surgery in comparison to conventional open surgery for colorectal cancer.
The indications of a right hemicolectomy include adenomatous polyps not suitable for removal by colonoscopy, inflammatory bowel disease, bleeding of arteriovenous malformations, obstruction, Crohn’s disease (and complications), ischemia, and any other condition for resection. Lesions can be resected from the ileum, mid-colon, and hepatic artery. Based upon recent reports in management of colon cancer, malignant disease can be treated safely including palliative resection for incurable carcinoma and potentially curable entities.
This is a very important issue for a successful result in laparoscopic colon resection. A thorough history and physical examination with special emphasis on cardiac and pulmonary problems as well as previous surgeries is mandatory. The patient and the operating team must be adequately informed of, and familiar with, the laparoscopic procedure. The patient should be informed that there is a possibility that the laparoscopic procedure may have to be converted to an open procedure.
It is very important to perform a complete workup of the colon to allow preoperative localization of the tumor by means of a barium enema, computed tomography (CT) scan, or colonoscopy with India ink marking where indicated. A baseline chemical profile including complete blood count, carcinoembryonic antigen, preoperative electrocardiogram, and chest radiograph should be performed as needed. The cardiac and pulmonary status of the patient should be very carefully evaluated to ascertain the patient’s ability to withstand a potentially longer procedure with abdominal distention and often a steep Trendelenburg and exaggerated lateral postures with increased pressure on the diaphragm. The bowel preparation must be modified from normal bowel preparation, as GoLYTELY frequently gives inadequate preparation and leaves increased fluid in the small bowel limiting visualization field. The authors recommend 5 days prior to surgery a low-fiber
diet, 3 days prior a full liquid diet, and 2 days prior clear liquids, adding 4 tablespoons of Milk of Magnesia in the middle of the day and another 4 tablespoons 6 hours later. The day prior to surgery, we recommend continuing with clear liquids and magnesium citrate (60 mL PO q12 h), with saline enema 6 hours and 2 hours previous to surgery. This uniformly results in a clean colon (mandatory for intracorporeal anastomosis and/or intraoperative colonoscopy, as well as monitoring fluid balance preoperatively and monitoring nutritional status). The patient is usually given IV antibiotics preoperatively; we prefer antibiotics that cover colon flora such as cefotaxime, metronidazole, or cefepime.
diet, 3 days prior a full liquid diet, and 2 days prior clear liquids, adding 4 tablespoons of Milk of Magnesia in the middle of the day and another 4 tablespoons 6 hours later. The day prior to surgery, we recommend continuing with clear liquids and magnesium citrate (60 mL PO q12 h), with saline enema 6 hours and 2 hours previous to surgery. This uniformly results in a clean colon (mandatory for intracorporeal anastomosis and/or intraoperative colonoscopy, as well as monitoring fluid balance preoperatively and monitoring nutritional status). The patient is usually given IV antibiotics preoperatively; we prefer antibiotics that cover colon flora such as cefotaxime, metronidazole, or cefepime.
Table 1 Monitor Positions | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Equipment
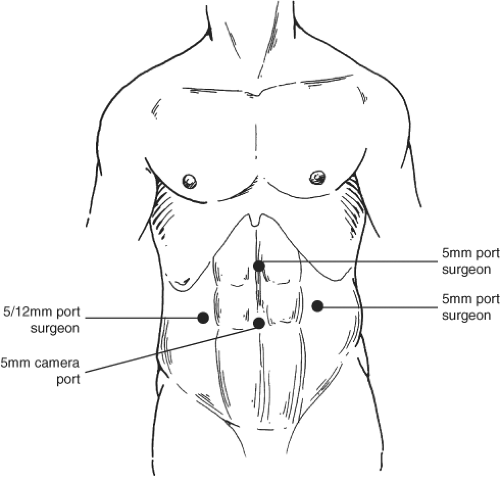
The equipment needed includes at least two monitors placed in accordance with the portion of the colon upon which the operation is planned as shown in Table 1. The operating table must allow for steep Trendelenburg positioning and for left and right tilting; additionally, anal access should be preferred for intraoperative colonoscopy when needed. Endoscopic staplers, 0- and 30-degree scopes, a three-chip high-resolution, high-definition video camera, and high-flow insufflator are very helpful. Trocars should be 5 mm, 10 mm, or universal 5/12 mm; these enhance the ability of a surgeon to place instruments of all sizes without changing reducers on the ports. A general rule is to “use as many trocars as needed” but our standard is four trocars. Generally, a half-circle around the target organ is the best setup for trocar placement, see Fig. 1. Standard graspers and special instruments including long bowel instruments, 5-mm laparoscopic scissors with cautery attachment, bipolar instrumentation, and those with cautery capabilities are needed, as are newer instruments for vessel control, such as the LigaSure coagulator or LigaSurge Advance (Valleylab, Boulder, CO). Clips or other devices may be used to control smaller blood vessels. An argon beam coagulator is helpful to control some but troublesome bleeding. Effective suction and irrigation devices (5 and 10 mm) with extra-long wands are recommended as well. Endo-GIA linear staplers with multiple reloads are in order.
An ultrasound device enhances evaluation of the liver as well as para-aortic nodes, and should be available when needed. Other instruments include special dissectors to dissect and free individual vessels. Laparoscopic bulldog Glassman clamps for vascular and bowel content control are frequently helpful. An instrument table for opening of the patient also needs to be immediately available, should occurrences arise that could demand an open procedure.
As part of the equipment needed in the surgical Endosuite, colonoscopy equipment is recommended. As discussed later in this chapter, the use of colonoscopy for laparoscopic colon resection is a must since it helps evaluate the anastomosis site and leaks as well as the presence of synchronous lesions.
Patient Positioning and Protective Devices
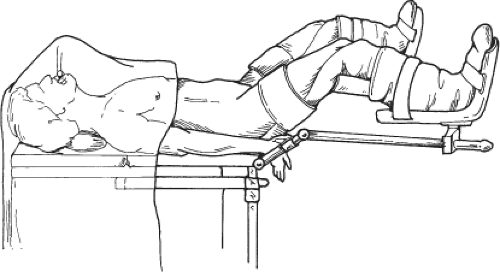
Correct patient positioning can greatly enhance a laparoscopic procedure. A supine position with ready anal access with the hips slightly flexed, 15 degree angle, aided by Lloyd-Davis or Allen stirrups and the buttocks near the edge of the table is extremely helpful (Fig. 2). We have found that taping the patient at the shoulders without restricting the pulmonary function is a very adequate method of stabilizing the patient for the airplaning positional changes and Trendelenburg that may be needed; however, bean bags and other restraining devices are also effective. Shoulder stripes or pads should be avoided as a sole means of preventing slippage as this can result in brachial plexus injury. It is also important to protect all exposed nerve surfaces, particularly those around the elbows and knees. The arms need to be secured by the patient’s side (if at all possible) to allow maximum tilt and mobility of the surgical team. As arms spread in the classic position will be an obstruction to movement around the operation table. Sequential compression devices are placed on the patient’s legs to help avoid venous stasis and an increased
risk of deep vein thrombosis. A warming blanket should be available to help prevent cooling of the patient, which most certainly can occur in longer procedures.
risk of deep vein thrombosis. A warming blanket should be available to help prevent cooling of the patient, which most certainly can occur in longer procedures.
Provisions should be made for warming of intravenous fluid and irrigation fluids as this can also be a source of patient cooling. We routinely use heparin (7,500 UI/L) in the irrigation fluid as this may be helpful in preventing large clots from forming as well as aiding in the reduction of tumor cell adhesion to instruments and trocars. With resections for cancer, povidone-iodine as an anticarcinogenic irrigation has been recommended to help reduce tumor cells and prevent tumor cell implantation on trocars and incisions. We tend to use this after the specimen is isolated or removed.
Warming the inspired gas is strongly recommended, and many authors recommend also warming the CO2, although no clear consensus is present for this. Wrapping the lower extremities in plastic bags is also recommended, and may prevent at least 1°C temperature loss per hour in a 2-hour or longer procedure. A Foley catheter and a nasogastric tube are routinely inserted.
Placing an arterial line and central line in any patient undergoing laparoscopic colorectal surgery is recommended, at the discretion of the anesthesiologist, particularly in the presence of cardiac and/or pulmonary compromise or with the expedition of a lower procedure.
It is very important to emphasize that before embarking upon laparoscopic colon resection of any type, the surgeon should have a proper background in advanced laparoscopy that includes intracorporeal suturing, intra-/extracorporeal knot tying, good use of both hands, and experience with stapling devices to avoid unneeded conversions to open procedures. Intricate knowledge of anatomic relationships between colonic vasculature, ureter, duodenum, superior mesenteric artery, stomach, common bile duct, kidney, and omentum is mandatory.
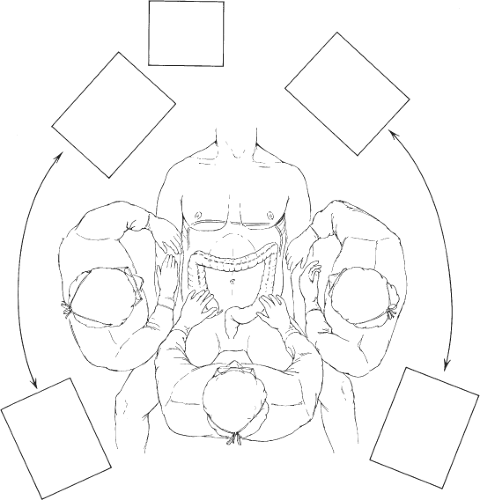
After prepping and draping the patient in sterile fashion, the surgeon and the camera operator stand to the patient’s left side, and the first assistant stands between the legs. A mobile video monitor is placed opposite the umbilicus to the patient’s right side, and another to the left, usually at the left shoulder to ensure that the entire surgical team has good visibility (Fig. 3).
Pneumoperitoneum is established by the use of Veress needle or Hassan technique, and the abdomen is insufflated with carbon dioxide gas to a pressure of 13 to 14 mm Hg. In most cases, the Veress needle is placed in the left mid flank; however, an alternate site, such as upper midline and left upper quadrant, is often selected in patients who have had prior abdominal surgery. Following adequate insufflation, a 5 port is placed on the left and a 5 mm 0-degree laparoscope is inserted. The abdomen is thoroughly inspected for signs of metastatic diseases or other disease processes, which may alter the anticipated procedure. Adhesions to the anterior abdominal wall are taken down carefully in a stepwise fashion, and the remainder of the working ports is placed under direct visualization. The
final configuration shows a 5-mm port in the upper midline, a 12-mm port in the right lower quadrant just below McBurney’s point, in addition to the 5-mm port in the left mid abdomen, and a 5-mm port at the umbilicus. Occasionally, additional ports may be placed in the left upper and right upper quadrants as needed. Once placed, the trocars are secured to the abdominal wall with a suture to prevent dislodgement and potential tumor infiltration in abdominal wall.
final configuration shows a 5-mm port in the upper midline, a 12-mm port in the right lower quadrant just below McBurney’s point, in addition to the 5-mm port in the left mid abdomen, and a 5-mm port at the umbilicus. Occasionally, additional ports may be placed in the left upper and right upper quadrants as needed. Once placed, the trocars are secured to the abdominal wall with a suture to prevent dislodgement and potential tumor infiltration in abdominal wall.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree