■ Combined multichannel intraluminal impedance and pH testing (MII-pH) detects episodes of reflux, regardless of the pH of the refluxate, by identifying changes inducted by the presence of liquids and gas in the esophagus. The episodes are classified as acid, weakly acid, or nonacid on the basis of concomitant pH monitoring. This test is useful in identifying bile reflux and does not require cessation of proton pump inhibitors for testing.
SURGICAL MANAGEMENT
■ A laparoscopic fundoplication is currently considered the procedure of choice for the treatment of GERD.
■ Even though several eponyms are used to describe different antireflux procedures, we believe that it is more important to focus on the technical elements that make a fundoplication effective and long lasting.
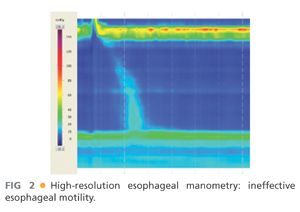
■ The type of fundoplication (total vs. partial) is tailored to the quality of esophageal peristalsis as documented by the preoperative manometry. In the United States, a partial fundoplication is proposed only to patients with very impaired or absent esophageal peristalsis in order to reduce the risk of postoperative dysphagia (FIG 2).
Preoperative Planning
■ A careful symptomatic evaluation testing is performed in every patient before surgical intervention.
Positioning
■ After induction of general endotracheal anesthesia, the patient is positioned in low lithotomy position with the lower extremities extended on stirrups with knees flexed 20 to 30 degrees. Alternatively, a split-leg table may be used.
■ To avoid sliding as a consequence of the steep reverse Trendelenburg position used during the entire procedure, a beanbag is inflated to create a “saddle” under the perineum.
■ Because increased abdominal pressure from pneumoperitoneum and the steep reverse Trendelenburg position decrease venous return, pneumatic compression stockings are always used as prophylaxis against deep venous thrombosis.
■ An orogastric tube is placed to keep the stomach decompressed during the procedure.
■ A Foley catheter is inserted at the beginning of the operation and removed at the end.
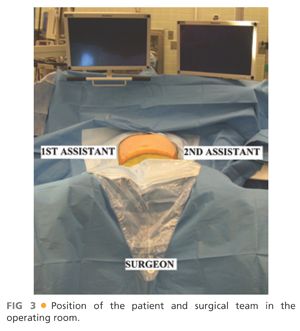
■ The surgeon stands between the patient’s legs. The first and second assistants stand on the right and left side of operative table (FIG 3).
TECHNIQUES
PLACEMENT OF PORTS
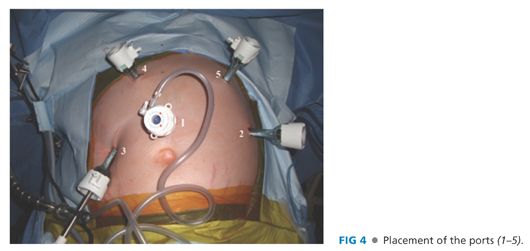
■ Five 10-mm trocars are used for the procedure (FIG 4).
■ The first incision is made in the midline 14 cm distal to the xiphoid process and a Veress needle is introduced into the peritoneal cavity. The peritoneal cavity is initially insufflated to a pressure of 15 mmHg. Subsequently, under direct vision, an optical port with a 0-degree scope (port 1) is placed. Once this port is placed, the 0-degree scope is replaced with a 30-degree scope and the other trocars are inserted under laparoscopic vision.
■ Port 2 is placed in the left midclavicular line at the same level of port 1. It is used by the assistant for traction on the gastroesophageal junction and to take down the short gastric vessels.
■ Port 3 is placed in the right midclavicular line at the same level of the other two ports. A retractor is used through this port to lift the left lateral segment of the liver to expose the gastroesophageal junction. The retractor is held in place by a self-retaining system fixed to the operating table.
■ Ports 4 and 5 are placed under the right and left costal margins so that their axes and the camera form an angle of about 120 degrees. These ports are used by the operating surgeon for the insertion of graspers, scissors, and dissecting and suturing instruments.
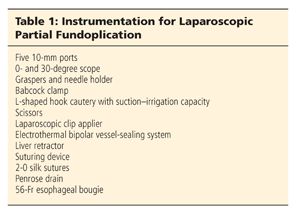
■ The instrumentation necessary for laparoscopic partial fundoplication is reported in Table 1.
DISSECTION
■ The gastrohepatic ligament is divided, beginning the dissection above the caudate lobe of the liver, where the ligament is thinner, and continuing toward the diaphragm until the right pillar of the crus is identified (FIG 5).

■ The right pillar of the crus is separated from the esophagus by blunt dissection until the left crus is recognized and the posterior vagus nerve is identified (FIG 6).
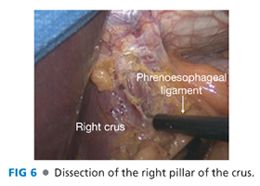
■ Subsequently, the peritoneum and the phrenoesophageal membrane overlying the esophagus are divided, and the anterior vagus nerve is identified.
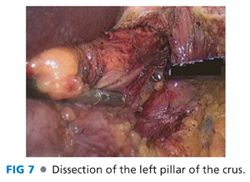
■ The left pillar of the crus is then separated from the esophagus and dissected toward the junction with the right pillar of the crus (FIG 7).
DIVISION OF THE SHORT GASTRIC VESSELS
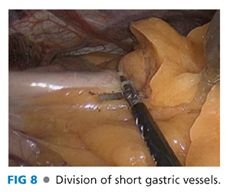
■ The short gastric vessels are taken down all the way to the left pillar of the crus, starting from a point midway along the greater curvature of the stomach (FIG 8).8
CREATION OF A WINDOW AND PLACEMENT OF A PENROSE DRAIN AROUND THE ESOPHAGUS
■ The esophagus is retracted upward with a Babcock clamp applied at the level of the esophagogastric junction.
■ A window is opened by a blunt and sharp dissection under the esophagus, between the gastric fundus, the esophagus, and the left pillar of the crus (FIG 9).
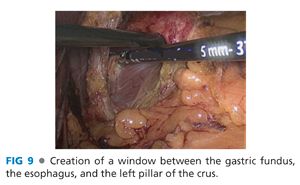
■ The window is enlarged, and a Penrose drain is passed around the esophagus.
■ Any hiatal hernia is completely reduced and a minimum of 3 cm of intraabdominal esophageal length is achieved.
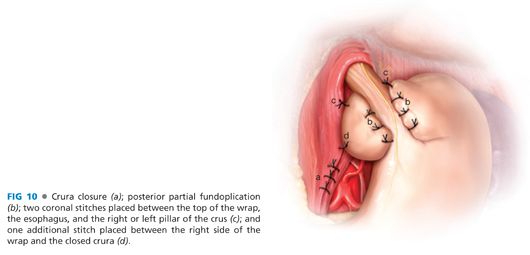
CLOSURE OF THE CRURA
■ Interrupted 2-0 silk sutures that are tied intracorporeally with an Endo Stitch device (Covidien, Norwalk, CT) are used to close the diaphragmatic crura (FIG 10a).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


