Laparoscopic Liver Resections
Ernesto P. Molmenti
George C. Sotiropoulos
Arnold Radtke
Charles Choy
Jeffrey M. Nicastro
Massimo Malagó
Gene F. Coppa
Background
The introduction of laparoscopic cholecystectomy was associated with an immediate reevaluation of many other surgical approaches. Never before had a surgical technique been accepted so widely in such a short time span. Together with this technical revolution, we also witnessed a “learning curve,” manifested by surgical complications associated with the training process.
Laparoscopic hepatic resections have the following advantages:
Are safe as demonstrated by multiple publications.
Are usually nonanatomic.
Constitute 20% to 80% of liver resections.
Close to 3,000 cases have been reported in the literature, both for benign and malignant tumors.
Have an associated morbidity of 10.5% and a mortality of 0.3%.
Have an incidence of positive margins no different than that of open resections.
Provide reduced postoperative pain, shortened recovery time, improved cosmetic results, and decreased length of hospital stay.
Can be performed on repeated occasions with good results.
As detailed below, there are three possible types of laparoscopic approaches. The choice should be based on the characteristics of the tumor, the status of the liver, the condition of the patient, and the experience of the surgeon. Most laparoscopic liver resections are nonanatomic.
Terminology and Types of Resections
There are three approaches to laparoscopic hepatic resections:
Pure laparoscopy (75% of cases)
Hand-assisted laparoscopy (17% of cases)
Hybrid technique (2% of cases)
The incidence of procedures performed includes:
Wedge resection or segmentectomy (45%)
Left lateral sectionectomy (20%)
Right hepatectomy (9%)
Left hepatectomy (7%)
Benign Asymptomatic Lesions
Laparoscopy is not currently viewed as a way to expand the surgical indications for benign hepatic lesions.
Colorectal Liver Metastases
When compared to open resection of liver metastases, the laparoscopic approach provided:
Comparable if not better oncologic outcomes
A greater incidence of negative margins
Comparable overall and disease-free survival rates
Less traumatic repeated resections
As in the case of open resections, patient selection and preoperative staging are vital in optimizing outcomes.
Hepatocellular Carcinomas
Laparoscopic resections for HCC:
Should follow (whenever possible) anatomical segmental boundaries since this has been shown to be associated with decreased recurrence rates.
Can assist in diagnosis, staging, and treatment.
Account for approximately half of laparoscopic liver cases.
When compared to open cases, laparoscopic HCC resections showed:
No difference in positive margins
No difference in disease-free or overall survival
Fewer adhesions
Decreased blood loss, operative time, and blood product requirements at the time of transplantation
Live Donor Hepatectomy
Laparoscopic live donor hepatectomy:
Remains the most controversial application of laparoscopic liver surgery.
A worldwide registry has been recommended.
Is a very delicate procedure, since both vascular inflow and outflow have to be maintained intact until the time of removal of the specimen in order to allow for the subsequent implantation. Live liver donation by itself is a procedure that should be performed only by very specialized centers. The additional complexity associated with a laparoscopic approach should be very cautiously considered.
Concomitant Procedures
Concomitant laparoscopic procedures at the time of laparoscopic hepatic resections:
Should have the same indications as in open procedures.
The safety and outcomes of both surgeries should be considered.
Usually include:
Radiofrequency ablation.
Colon resections.
Laparoscopic respectability is based on the following variables:
Characteristics of the tumor:
Etiology: benign/malignant:
The indications for laparoscopic resection are similar to those for open cases.
Benign tumors are (except in exceptional cases) resected when symptomatic or when malignancy cannot be excluded.
Malignant tumors are resected in the absence of untreatable extrahepatic disease that would shorten the otherwise expected survival.
Chemotherapy treatments (when indicated) should not undergo any changes due to the laparoscopic nature of the procedure.
Size and location:
Ideal for laparoscopic resection are tumors <5 cm located in segments 2, 3, 4, 5, and 6.
Tumors located centrally, in the posterior right lobe, at the hilum, at the resection margin, adjacent to major vessels, or whose resection requires vascular and/or biliary reconstructions may not be resectable laparoscopically.
Number of lesions:
The operating surgeon should determine based on each individual patient characteristics the numbers of tumors that can be resected.
Status of the liver:
Laparoscopy does not alter the risk associated with any preexisting liver dysfunction.
The presence of cirrhosis, fibrosis, steatosis, and other types of liver involvement should be carefully evaluated since such findings are associated with an increased incidence of complications.
Decompensated cirrhosis (like in the case of any open surgery except for liver transplantation) is associated with a usually unacceptable risk of morbidity and mortality.
Prior to performing any resection, the operating surgeon should verify that the remnant liver volume is both anatomically and physiologically adequate.
A tumor resectable from a technical point of view may not be resectable from a physiological perspective.
Parenchymal congestion associated with impaired venous outflow can be a source of physiological parenchymal compromise in the setting of seemingly adequate anatomical volume.
Condition of the patient:
Laparoscopy does not eliminate the physiologic stress and risks associated with major resections.
Patients should be able to tolerate the procedure from an overall physiological point of view.
Cardiovascular and pulmonary preoperative evaluation is necessary.
Experience of the surgeon:
Major hepatic resections should be undertaken only by highly experienced surgeons.
There is a learning curve associated with laparoscopic resections.
Preoperative workup includes:
Abdominal and pelvic imaging studies (usually ultrasound, CT, and/or MRI)
Chest imaging (CT and/or x-ray)
Clinical biochemistry studies
Cardiology evaluation
Other clearances as needed
In instances of possible cirrhosis based on clinical, imaging, and biochemical findings, a liver biopsy can be a helpful aid in establishing the underlying status of the liver. Liver biopsy (when not contraindicated) should also be considered in cases of uncertain pathologies.
When indicated, portal vein embolization is usually undertaken 3 weeks prior to the planned resection in order to augment the volume of the remaining hepatic parenchyma. The absence of enlargement of the nonembolized liver is a sign of concern, since it could be a sign of liver injury such as fibrosis or cirrhosis.
We offer patients the option for autologous blood donation prior to the procedure.
The procedure should be thoroughly discussed and adequate preoperative consent obtained preferably by the attending surgeon. Patients should be made aware of risks and benefits, as well as of potential complications and their treatment.
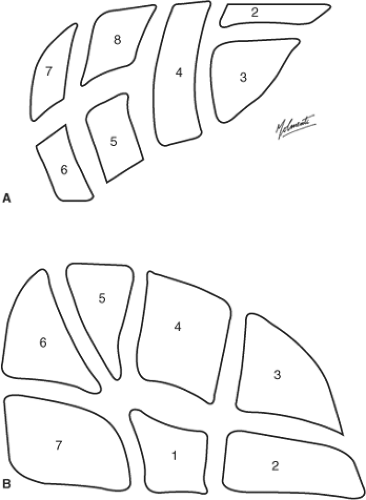
Thorough knowledge of liver vascular and biliary anatomy is essential (Figs. 1–5). The use of three-dimensional computer-assisted planning (such as HepaVision, MeVis, Germany) allows us to perform virtual resections prior to the procedures (Figs. 6–9). It also provides us with information on vascular inflow/outflow patterns and safely perfused/drained retained liver volumes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree