■ The left arm is left out at a 75-degree angle and secured to the arm board with a gauze wrap. If the patient’s body habitus allows, the right arm is ideally tucked at the side. The bed is positioned down as low as possible.
■ A standing stage is placed on the patient’s right side to be used by the operating surgeon. The assisting surgeon stands on the patient’s left side.
■ A 34-Fr gastric lavage tube is placed in the patient’s stomach and allowed to drain. A glove may be placed at the end of the lavage tube to prevent spillage of gastric contents. No other devices except the gastric lavage tube and endotracheal tube should be in the patient’s mouth.
TECHNIQUES
PLACEMENT OF INCISIONS
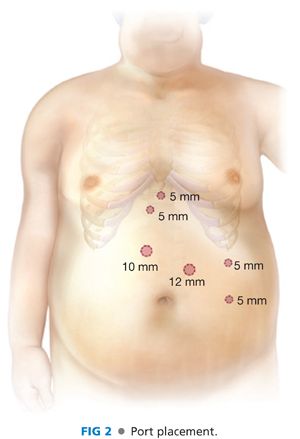
■ Sixteen centimeters is measured down in the left paramedian position. The skin and underlying fascia is injected with local anesthetic, and a 10-mm visual port is inserted through the left rectus sheath, identifying all layers of the abdominal wall. Pneumoperitoneum is then established. An inspection of the abdomen and pelvis is then performed ensuring there was no injury from the initial trocar placement.
■ The remaining five ports are then placed. The first 5-mm trocar is placed just inferior to the xiphoid process and to the left of the falciform for liver retraction. A second 5-mm trocar is placed approximately 2 cm to the right and inferior to the first 5-mm trocar placement. This 5-mm right paramedian port is also placed to the left of the falciform. A 12-mm right paramedian trocar is placed to the left of the falciform approximately one handbreadth from the second 5-mm trocar. A 5-mm left subcostal trocar is placed 2 cm below the costal margin. A final 5-mm trocar is placed 1 or 2 cm below the level of the initial port, as far lateral as possible (FIG 2).
LIVER BIOPSY
■ A needle biopsy of the liver is obtained because blood tests do not accurately predict the presence, absence, or degree of histologic changes due to fatty liver disease. The liver is elevated by two bowel graspers placed through the left lateral ports to ensure the biopsy needle does not go through the liver and cause injury to underlying structures. Two core biopsies are obtained from the left lateral segment of the liver for pathologic examination for the diagnosis and staging of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH).
LIVER RETRACTION
■ The patient is placed in full reversed Trendelenburg position. The liver is retracted with a locking Allis grasper clamp placed through the subxiphoid 5-mm port and secured to the diaphragm just anterior to the gastroesophageal (GE) junction (FIG 3).

GASTRIC POUCH CREATION
■ With the gastric lavage tube retracted into the esophagus by the anesthetist, the angle of His is exposed and dissected with an ultrasonic dissector.
■ Identification, dissection, and primary posterior repair of a hiatal hernia is done at this time, if necessary. Five centimeters is measured down from the GE junction along the lesser curve where the lesser sac is entered immediately adjacent to the lesser curve of the stomach using the ultrasonic dissector to divide branches of the left gastric artery.
■ A 45-mm laparoscopic stapling device with appropriate-sized staples is oriented transversely to the lesser curve and fired.
■ The 34-Fr gastric lavage tube is advanced to abut this newly placed horizontal staple line. Additional firings of laparoscopic stapling devices are placed parallel to the lavage tube. Complete transaction of the stomach and hemostasis are ensured by inspecting the entire staple line. Once divided, the gastric lavage tube is retracted back into the esophagus.
■ The retrogastric and pancreatic adhesions are freed using the ultrasonic dissector to increase pouch mobility (FIG 4).

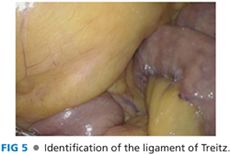
IDENTIFICATION OF THE LIGAMENT OF TREITZ
■ The table is taken out of reversed Trendelenburg and placed in the supine position. The omentum is retracted cephalad, exposing the transverse mesocolon, which is also elevated and retracted cephalad. The proximal jejunum is retracted to expose the ligament of Treitz and the inferior mesenteric vein (FIG 5).
CREATION OF THE BILIOPANCREATIC LIMB
■ Starting at the ligament of Treitz, a marked grasper in the surgeon’s right hand is used to measure 40 cm distally (FIG 6).

■ The jejunum is divided with a white 60-mm laparoscopic stapling device, with care being taken not to undercut the biliopancreatic or Roux limb mesentery.
■ If necessary, further mesenteric division can be accomplished with an ultrasonic dissector.
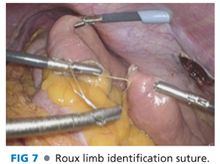
JEJUNOJEJUNOSTOMY CREATION
■ A 2-0 undyed absorbable suture is placed on the tip of the distal jejunum to later identify the Roux limb (FIG 7). The Roux limb is measured using the previous technique with a marked grasper in the surgeon’s right hand. A 95-cm Roux limb is created if the patient’s BMI is less than 50. A 150-cm Roux limb is created if the patient’s BMI is greater than 50.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


