Langerhans Cell Histiocytosis in Bone Marrow
Key Facts
Clinical Issues
2 major groups
Single-system Langerhans cell histiocytosis
Single site disease (unifocal lymph node, skin, lung, pituitary, or bone)
Multifocal disease (multifocal bone or multiple lymph nodes)
Multi-system Langerhans cell histiocytes
2 or more organs involved at diagnosis without organ dysfunction
2 or more organs involved at diagnosis with organ dysfunction
High risk: Involvement of 1 or more risk organs (liver, lung, spleen, or hematopoietic system)
Low risk: Involvement of other organs
Microscopic Pathology
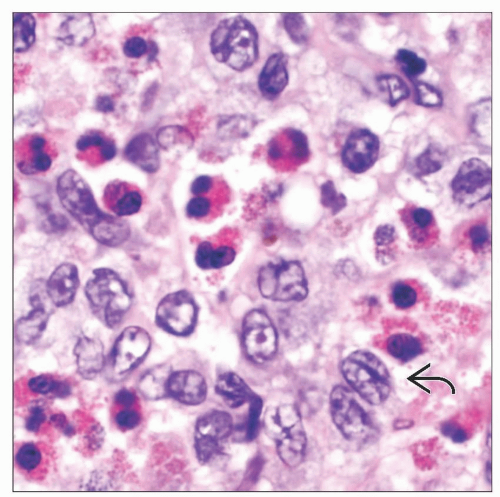
Bone marrow findings
Patchy clusters of Langerhans cells often associated with variable numbers of eosinophils
Marrow involvement may be associated with fibrosis
Langerhans cells may also be occasionally detected on marrow aspirate smears
Bone marrow trephine biopsy is preferred to aspirate due to higher yield
Ancillary Tests
Expression of CD1a, langerin, and S100
Intracytoplasmic, tennis racquet-shaped Birbeck granule by electron microscopy
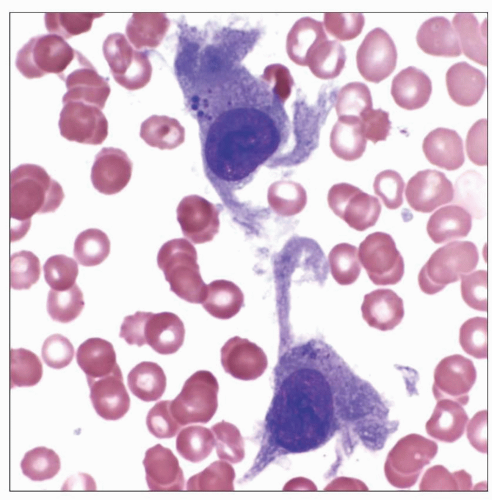 Wright-stained bone marrow aspirate smear from an infant with Langerhans cell histiocytosis demonstrates 2 Langerhans cells with elongated dendritic projections. |
TERMINOLOGY
Abbreviations
Langerhans cell histiocytosis (LCH)
Synonyms
Histiocytosis X, eosinophilic granuloma (solitary lesion)
Hand-Schüller-Christian disease (multiple lesions)
Letterer-Siwe disease (disseminated disease or visceral involvement)
Definitions
Nonneoplastic Langerhans cells (LC)
First described by Paul Langerhans in 1868
Bone marrow-derived antigen-presenting cells
Normally reside in mucosal sites and epidermis
Migrate to lymph node following antigenic stimulation
Langerhans cell histiocytosis
Clonal proliferation of LCs in all forms except smoking-related pulmonary LCH
Morphologic, immunophenotypic, and ultra-structural features are similar to nonneoplastic LCs
ETIOLOGY/PATHOGENESIS
Etiology Remains Poorly Understood
Documented affected relative in 1% of patients
Higher rate of concordance for LCH in monozygotic (92%) vs. dizygotic (10%) twins
Reported chromosomal instability and loss of heterozygosity on chromosomes 1, 4, 6, 7, 9, 16, 17, and 22
No apparent genomic aberrations in some studies
CLINICAL ISSUES
Epidemiology
Incidence
8-9 cases per 1,000,000 in children
1-2 cases per 1,000,000 in adults
Gender
More common in males (M:F ratio 3.7:1)
Site
2 major groups (per Histiocyte Society)
Single-system Langerhans cell histiocytosis
Single site disease (unifocal lymph node, skin, lung, pituitary, or bone)
Multifocal disease (multifocal bone or multiple lymph nodes)
Multi-system Langerhans cell histiocytosis
2 or more organs involved at diagnosis without organ dysfunction
2 or more organs involved at diagnosis with organ dysfunction
High risk: Involvement of 1 or more risk organs (liver, lung, spleen, or hematopoietic system)
Low risk: Involvement of other organs
Presentation
Symptoms depend on site infiltrated by LCH
Fracture due to osteolytic lesion, and pain
Variable clinical presentation
Bone LCH
Most commonly affected organ
Often single skull lesion in affected children
Cutaneous LCH
Typically presents with eczematous rash
Pulmonary LCH
Dry cough and dyspnea on exertion common
Constitutional symptoms may occur
Incidental x-ray finding in about 25% of asymptomatic patients
In children and infants, commonly part of a multi-system LCH
In young adults, mainly isolated pulmonary LCH
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree