Langerhans Cell Histiocytosis
Key Facts
Terminology
Proliferation of Langerhans cells that form multiple interstitial, bilateral, peribronchiolar pulmonary nodules
Clinical Issues
Highest incidence is in cigarette smokers (95% of patients)
18-40 years
Predominantly affects upper and mid zones of the lungs
Asymptomatic in approximately 15% of patients
Microscopic Pathology
Interstitial proliferation of Langerhans cells distributed along small airways (bronchioles and alveolar ducts)
Larger lesions produce stellate-shaped or round nodules around bronchioles
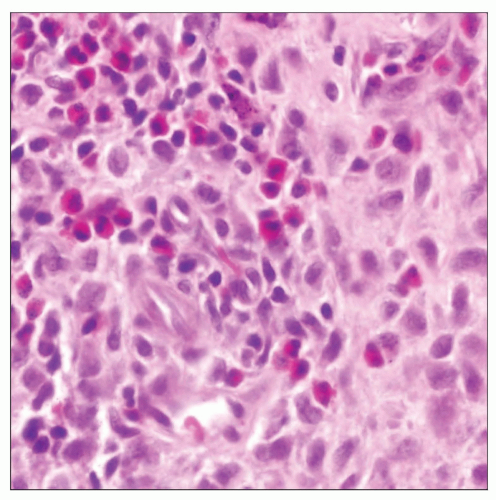
Lesions may be paucicellular or contain abundant Langerhans cells
Nodular lesions may show cystic changes and cavitation
Langerhans cells show round to oval nuclei with frequent nuclear irregularities and nuclear infolding (grooves)
Langerhans cells are accompanied by abundant eosinophils
Ancillary Tests
Langerhans cells are positive for S100 protein and CD1a
Zipper-like structures (Birbeck granules) are pathognomonic on electron microscopy
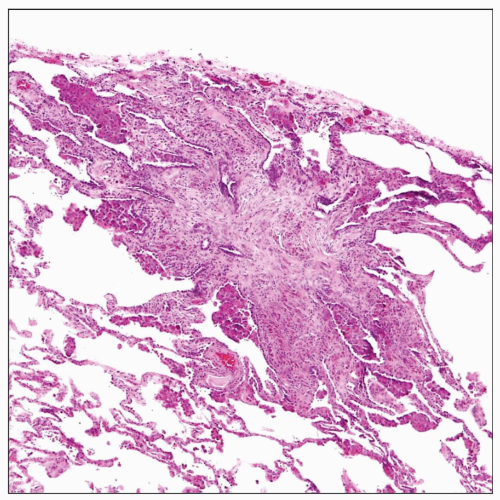 Histologic appearance of a focus of Langerhans cell histiocytosis shows a stellate-shaped area in the periphery of the lung with sparse cellular proliferation. |
TERMINOLOGY
Abbreviations
Langerhans cell histiocytosis (LCH)
Synonyms
Eosinophilic granuloma, Langerhans cell granulomatosis, histiocytosis-X
Definitions
Proliferation of Langerhans cells that form multiple interstitial, bilateral, peribronchiolar pulmonary nodules
ETIOLOGY/PATHOGENESIS
Pathogenesis
Clonality studies in the lung have suggested both reactive and neoplastic process
95% of patients are cigarette smokers, suggesting link with cigarette smoking
CLINICAL ISSUES
Epidemiology
Incidence
Highest incidence is in cigarette smokers (95% of patients)
Age
18-40 years
Gender
Slight male predominance
Site
Predominantly affects upper and mid-zones of lungs
Presentation
Cough
Dyspnea
Chest pain
Systemic symptoms (malaise, fever, weight loss)
Extrapulmonary involvement seen in 15% of patients
Asymptomatic in approximately 15% of patients
Laboratory Tests
Pulmonary function tests show restrictive disease with decreased diffusing capacity
Natural History
Some patients may experience spontaneous remissions while others may progress to end-stage pulmonary fibrosis
Disease often regresses with cessation of smoking
Treatment
Steroids
Cessation of smoking
Immunosuppressive therapy in refractory cases
Spontaneous resolution in some cases