9 Kidney and Urinary Tract Disease
Presentation of kidney and urinary tract disease
• Patients’ complaints are directly related to the urinary tract or urine output, e.g. frequency, dysuria, burning micturition, urgency, colic, polyuria, nocturia, haematuria, oliguria, and anuria.
• Discovery of abnormal laboratory findings during routine investigations, e.g. proteinuria, haematuria, elevated plasma creatinine, electrolyte and acid–base disturbances.
• Symptoms and signs of renal failure (e.g. uraemia, anaemia, anuria, hypertension and oedema) in the absence of prior renal disease.
• Discovery of renal and urinary tract disease as part of involvement in systemic disease, for example:
Information
Fluid balance and electrolytes: assessing fluid status
Clinical assessment
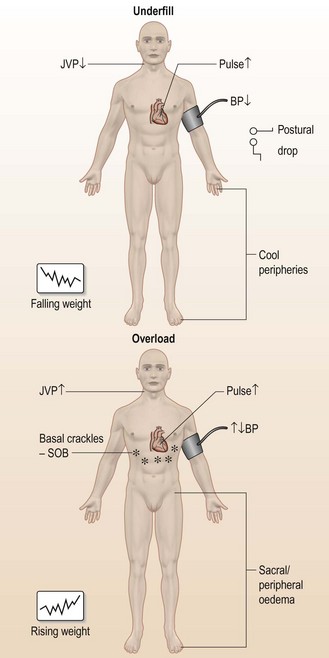
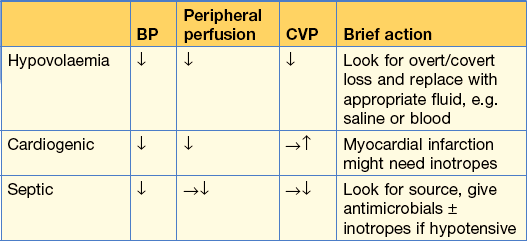
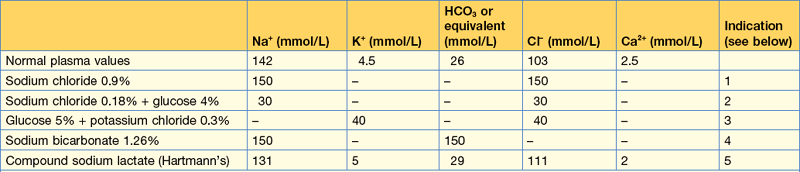
Take a quick history, particularly of fluid and electrolyte intake (oral or intravenous) and output (renal, GI tract or skin), then examine the patient (Fig. 9.1, Table 9.1).
Table 9.1 Tools to assess fluid status
| Useful | Not so useful | |
|---|---|---|
| Clinical examinations | BP (especially postural or post-exercise drop) | Skin turgor |
| Oedema | Eye turgor | |
| JVP | Mucous membranes | |
| Peripheral perfusion | ||
| Pulse | ||
| Basal crackles | ||
| Charts | Serial weight (on same machine) | Fluid balance (input/output) |
| Additional tools | CVP line – use dynamically | CVP – absolute |
| CXR | Urine Na+ | |
| Pulmonary artery flow catheter | Osmolality |
Case history (1)
He is normally fit and well and he wonders whether he has some form of severe gastroenteritis.
Figure 9.1 (a) shows the other signs of hypovolaemia.
Investigations
Management
An emergency CT scan confirmed the haemothorax and an intercostal tube drain was inserted.
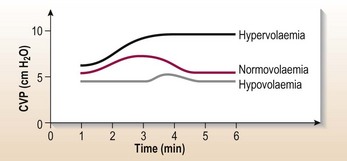
A CVP line was inserted to assess fluid balance. Fluid challenge (Table 9.2 and Fig. 9.2) indicated hypovolaemia, and blood transfusion (2 units) was started with repeated checks on his fluid status.
A laparotomy was performed and 20 cm of small bowel resected.
Fluid balance and electrolytes: sodium problems
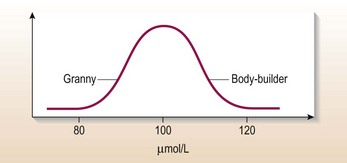
What are you actually measuring when you measure the serum sodium?
Using this concept you can describe how serum Na+ becomes abnormally low (hyponatraemia) or high (hypernatraemia) (Table 9.3).
Table 9.3 Hyponatraemia and hypernatraemia
| Ratio (Na+ : water) | Extracellular water |
|---|---|
| Hyponatraemia | |
| Water ↑ | → or ↓ |
| Water ↑ > Na+ ↑ | ↓↓ |
| Na+ ↓ | ↓ |
| Hypernatraemia | |
| Water ↓ | → or ↓ |
| Water ↓ > Na+ ↓ | ↓↓ |
| Na+ ↑ | ↑ |
How do I work out why?
The key is to determine the extracellular water. Examine the patient (see Fig. 9.1).
Management
On examination there were no features of fluid depletion, which excludes true Na+ depletion.
Action
• Stop IV fluids, restrict oral fluids to 1 litre daily and food as requested by the patient. 48 hours later her serum sodium is 132 mmol/L.
Other causes of hyponatraemia
• Diuretic therapy: particularly loop diuretics cause large renal losses of salt and water and metabolic alkalosis.
• Severe heart failure, advanced liver cirrhosis or nephrotic syndrome: hyponatraemia with increased total body sodium and even greater excess of water resulting in ascites and oedema. Plasma osmolality is low. Increased water orally continues in the face of salt restriction, diuretic therapy or both and will aggravate the ascites and oedema.
• Syndrome of inappropriate ADH production (p. 459).
• Pseudohyponatraemia: e.g. hyperlipidaemic states where sodium is confined to the aqueous phase or monoclonal gammopathies, hyperglycaemia (10 mmol rise reduces sodium by approximately 2 mmol).
Hypernatraemia
Hypernatraemia is defined as sodium > 145 mmol/L.
• Iatrogenic: IV infusion of hypertonic sodium bicarbonate, hyperalimentation by IV route or nasogastric tube, sodium chloride tablets, sea water drowning or mineralocorticoid excess; total body sodium is elevated in these conditions. Signs are of hypervolaemia.
• Impaired thirst/unconscious patient: total body sodium is low because of both sodium and water deficit but water losses are greater than the losses of sodium. Signs are of hypovolaemia.
• Osmotic diuresis, e.g. diabetic ketoacidosis, radiocontrast, mannitol: total body sodium is low because of both sodium and water deficit, but water losses are greater than sodium losses. Urine is not maximally concentrated despite hyperosmolar state, in contrast to GI losses of sodium and water where urine is maximally concentrated. Signs here are of hypovolaemia.
• Water loss, e.g. diabetes insipidus: normal total body sodium. Signs are of euvolaemia.
Treatment
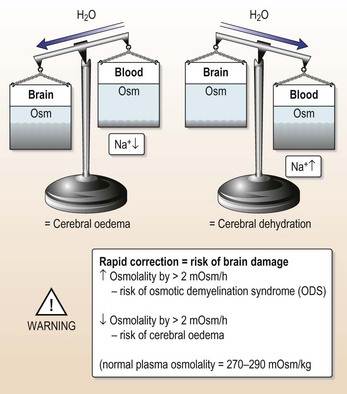
• Avoid rapid correction (Fig. 9.3). Serum Na+ should not fall > 1 mmol every 2 hours, i.e. 10 mmol/24 hours.
• Initially give IV 0.45% saline. This is followed by 5% glucose with 20 mmol/L K+ with frequent monitoring of volume status and serum Na+ level. This stays in the extracellular compartment (see assessing fluid status, p. 223).
Patient stopped passing urine
What should you do?
Take a detailed history of type of surgical procedure. Ask about GI bleeding, dehydration or other fluid losses, nephrotoxic drugs, drugs associated with hypersensitivity reaction causing tubo-interstitial nephritis (e.g. penicillins, NSAIDs, cephalosporins), evidence of previous renal insufficiency, and any radiological procedure with contrast enhancement. Anuria usually means obstructive uropathy or vasculitides rather than acute tubulo-nephritis (ATN); evidence of these conditions should be sought.
On examination the patient has a tachycardia of 110 bpm with a low BP 90/50.
Common causes of poor urinary output
• Urine retention: always catheterise.
• Dehydration: assess fluid status (see Fig. 9.1). Look at fluid balance charts.
Initial management
This man is fluid depleted and needs fluid replacement (Table 9.5):
• 0.9% saline IV ( 20 mmol/K+) added to each litre
• Write up initial regimen: modulate according to patient age, size and severity
• Reassess fluid status regularly
Still no urine?
• Are you certain the patient is adequately fluid replete?
• Check that the urine catheter is not blocked or misplaced.
• Give a loop diuretic, e.g. furosemide.
• The patient might now have established acute kidney injury. Refer to nephrologist.
Fortunately this man responded to fluid replacement and produced urine, intitially 50 mL/hour.
Acute heart failure
What has gone wrong?
RIFLE criteria for acute kidney injury
| Grade | GFR Criteria | UO Criteria |
|---|---|---|
| Risk | SCr × 1.5 or GFR decrease >25% (within 48 hr) | UO < 0.5 mL/kg/h × 6 h |
| Injury | SCr × 2 or GFR decrease >50% | UO < 0.5 mL/kg/h × 12 h |
| Failure | SCr × 3, GFR decrease >75%, | UO < 0.3 mL/kg/h × 24 h |
| SCr > 350 µmol/L | ||
| with an acute rise > 40 µmol/L | ||
| Loss | Persistent AKI > 4 weeks | |
| ESKD | Persistent ESKD > 3 months |
SCr = serum creatinine; UO = Urinary output; ESKD = end stage kidney disease.
(Bellomo R, Kellum JA, Ronco C. Acute kidney injury. Lancet 2012; 380: 756–766.
There is a new consensus definition that merges RIFLE criteria and the Acute Kidney Injury network definition (Kidney Disease Improving Global Outcomes (K-DIGO) group 2012).
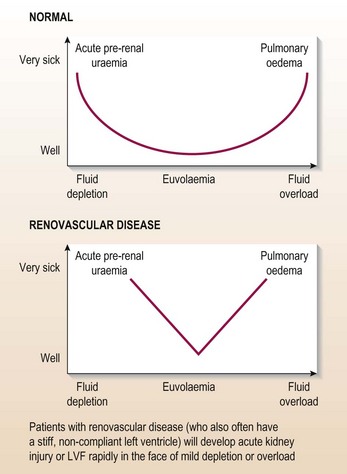
Clinical suspicion of renovascular disease
• Most patients will have disseminated atheroma with missing pulses and/or bruits and a history of smoking.
• Abdominal/renal bruits (although they have a very strong association with renal artery stenosis (RAS)) are rare.
• ‘Flash pulmonary oedema’ (without an obvious precipitant) is a good predictor of renovascular disease.
• Brittle response to volume loading or off-loading (Fig. 9.5).
Note: her renal function was abnormal at presentation.
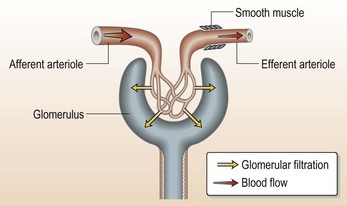
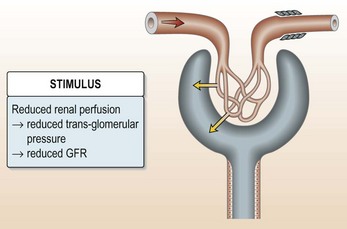
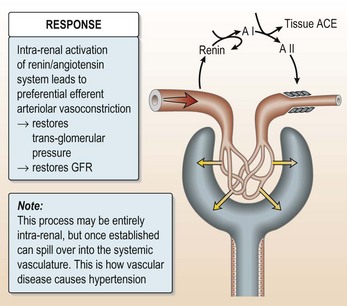
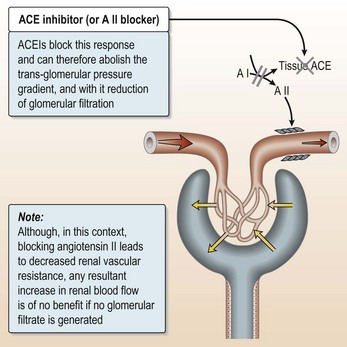
ACE inhibitors can cause acute kidney injury in patients with renovascular disease (Fig. 9.6).
How should patients like this be managed?
The key to successful management is very careful fluid control.
Managing acute heart failure (AHF) in the presence of suspected renovascular disease
• Treat the pulmonary oedema: it is a dangerous and very distressing condition.
• Avoid ACEIs/AII blockers: use other vasodilators (this patient was given captopril!).
• Avoid rapid volume off-loading: titrate the diuretic dose against renal function.
• Insert a CVP line and use it properly (see Fig. 9.1).
• Examine (and weigh) the patient regularly: use low-dose dopamine (can be given via peripheral line at 2.5 mg/kg/min) for its natiuretic effect if no response to initial therapy.
Renal imaging investigations
• Ultrasound: unequal renal size (> 2 cm difference) is a good predictor of renovascular disease but its absence does not exclude RAS. Duplex ultrasound is used to demonstrate renal artery perfusion.
• Isotope renography: unequal function, slow transit and altered dynamics with captopril are all suggestive of renovascular disease. In experienced hands and with good renal function, its sensitivity and specificity are 70% (creatinine < 150 µmol/L); however, in inpatients with severe renal impairment its sensitivity falls below 30%.
• MR angiography is increasingly used to visualise the renal arteries.
• Intra-arterial angiography: the gold standard – should be done by experienced radiologists with minimal contrast load.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree