Jejunostomy Tube
Rebecca L. Wiatrek
Lillian S. Kao
DEFINITION
A jejunostomy feeding tube is a tube placed into the proximal jejunum and brought out through the skin to allow for feeding distal to the stomach. Jejunostomy tubes are indicated in patients who are unable to maintain adequate nutrition orally and who are unable to be fed via the stomach. Examples of conditions that may require a jejunostomy tube include, but are not limited to, gastric outlet obstruction, esophageal perforation, gastroparesis, or recurrent aspiration. Jejunostomy tubes may be placed via a nasojejunal or percutaneous route; the latter can be approached via interventional radiology, via laparoscopic or open surgery, or via endoscopy, as an extension through a percutaneous gastrostomy tube.
PATIENT HISTORY AND PHYSICAL FINDINGS
A complete surgical history should be elicited, focusing on prior abdominal operations.
A complete abdominal examination should be performed, noting prior incisions and hernias.
Because malnutrition may be an indication for placement of a jejunostomy tube, a complete nutritional history should be obtained including recent weight loss.
Physical examination should be focused on signs of severe malnutrition such as loss of subcutaneous fat, muscle wasting, and/or presence of edema and ascites.
The Subjective Global Assessment Score combines the history and physical examination to provide a rating from A (well nourished) to C (severely malnourished).
IMAGING AND OTHER DIAGNOSTIC STUDIES
A nutritional assessment should be performed. Severe malnutrition may be a reason for placement of a jejunostomy tube, such as prior to major elective surgery. Indicators of preoperative malnutrition include weight loss greater than 10% to 15% over the previous 6 months, body mass index less than 18.5 kg/m2, Subjective Global Assessment Grade C, and/or serum albumin less than 3 g/dL.1
Electrolytes should be checked and replaced prior to surgery. An electrocardiogram should also be checked in order to rule out cardiac abnormalities and arrhythmias.
Additional studies and radiologic imaging should be based on the primary diagnosis. In patients with underlying malignancy, staging studies should be recent enough to ensure that there are no changes in the cancer status that may affect the operative plan.
SURGICAL MANAGEMENT
Preoperative Planning
Although enteral feeding is preferred to the parenteral route, the surgeon should ensure that there are no contraindications to enteral nutrition such as distal obstruction, ileus, highoutput enterocutaneous fistula, or shock. Alternatives to jejunostomy tubes include temporary nasally inserted feeding tubes and gastrostomy tubes. Temporary feeding access can be achieved using a nasogastric or a nasojejunal feeding tube; the latter can be placed with the assistance of fluoroscopy or endoscopy. Smaller diameter feeding tubes may be more comfortable for the patient but also may be more prone to clogging. Gastrostomy tubes for longer term feeding access can be placed endoscopically, radiologically, or surgically.
If enteral access is not the primary indication for surgery, then the complete operative plan should be considered. The anticipated duration of inability to take in oral nutrition or of inadequate nutrition (<60% of caloric requirement) should be taken in consideration when deciding whether or not to place a feeding jejunostomy tube as well as in deciding the route of placement (nasojejunal vs. surgical).1 In cancer patients, whether the goal of surgery is curative or palliative should be considered. A temporary feeding jejunostomy tube may be indicated after resection of cancer of the esophagus, stomach, or pancreas to allow continued distal enteral nutrition in the event of an anastomotic leak.
Palliative care may include placement of a surgical jejunostomy tube. Cancer patients who are not candidates for curative treatment should be assessed for their preferences, quality of life, and resources. The risks of surgical intervention should be weighed against the potential benefits of enteral nutrition. A candid discussion should be held with the patient regarding advanced directives and end-of-life care.
When enteral access is the primary indication for surgery, the surgeon should discuss the planned operative approach with the patient. When a laparoscopic jejunostomy tube is planned, the surgeon should discuss the possibility of conversion to open. If the jejunostomy tube is palliative, the surgeon should discuss the possibility of aborting the procedure when the risks outweigh the benefits (i.e., in the setting of carcinomatosis and inability to safely dissect the proximal jejunum).
Although no randomized trials exist regarding antibiotic prophylaxis prior to jejunostomy tube placement, there is high-quality evidence that antibiotic prophylaxis reduces surgical site infections across procedures and baseline risks.2 In addition, a meta-analysis of randomized controlled trials of antibiotic prophylaxis to prevent peristomal infection after percutaneous endoscopic gastrostomy demonstrated a significant risk reduction with cephalosporin and penicillinbased prophylaxis.3
Positioning
The patient should be positioned in the supine position. This is required for both laparoscopic and open techniques. For the laparoscopic approach, it is important to secure the patient to the bed with straps or tapes to allow for safe manipulation of the operating table.
TECHNIQUES
OPEN JEJUNOSTOMY FEEDING TUBE PLACEMENT
First Step—Placement of Skin Incision
A limited midline incision, approximately 5 cm in length, is made above the umbilicus. This allows for identification of the ligament of Treitz. A larger incision may be needed if the patient has had multiple prior operations requiring adhesiolysis.
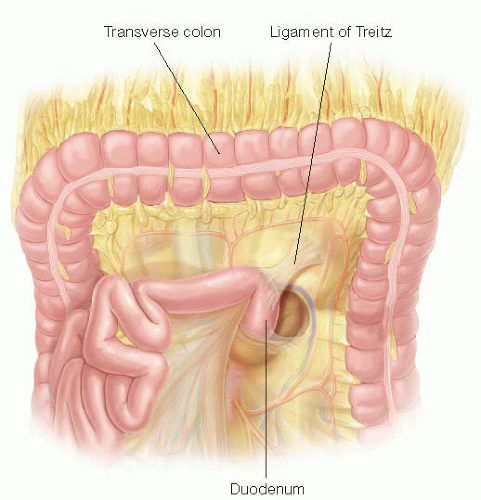
Once the abdomen is entered, the omentum can be followed to the transverse colon, which is retracted cephalad. The ligament of Treitz is located at the base of the transverse mesocolon to the left of the fourth portion of the duodenum (FIG 1) and is identified by visualization and palpation. A segment of jejunum distal to the ligament of Treitz is identified. A distance of 15 to 20 cm from the ligament of Treitz will allow the jejunum to reach the abdominal wall without tension, while also providing for enough length for a proximal revision of the jejunal segment, should one be necessary in the future.
An exit site is identified in the skin of the left upper quadrant, several centimeters lateral from the midline. A stab incision is made at this level, and tonsil clamps are used to deliver the jejunostomy tube into the abdominal cavity.
Second Step—Choice of Tubes
The type of jejunostomy tube used can be as simple as a 10-or 12-French red rubber catheter or a silicone jejunostomy tube similar to those used in laparoscopic cases. Silicone tubes may have more longevity.4 Avoid using balloontipped catheters (i.e., Foley catheters) or, alternatively, ensure that the ability to inflate the balloon has been disabled to prevent future attempts at insufflating the balloon that could lead to subsequent bowel obstruction.
If using a red rubber catheter, the tip may be cut off, which allows for exchange over a wire should the tube become clogged. Additional side holes may also be cut at the distal end of the tube in order to improve flow through the catheter.
Third Step—Suturing Tube into the Bowel
The previously chosen site of proximal jejunum is delivered into the wound. The site of entry of the tube should be on the antimesenteric side of the jejunum. Once this is identified, a 3-0 silk is used to create a diamond-shaped purse-string suture. A small opening is made inside the purse-string suture with cautery, only large enough to allow for the tube to be inserted into the bowel.
The tube is placed into the bowel and advanced into the distal portion of the jejunum. The length of advancement into the jejunum should be long enough to prevent backflow of feeds into the proximal small intestine.

FIG 2 • The open Witzel technique. 3-0 silk seromuscular sutures are placed perpendicularly on the antimesenteric border of the bowel on both sides of the feeding tube (Lembert sutures) in order to imbricate the bowel wall over the feeding tube, creating a serosal tunnel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access