12 ITU
Shock
Case history (1)
On examination he is pale and clammy. His pulse is 100/min, poor volume and BP 90/60.
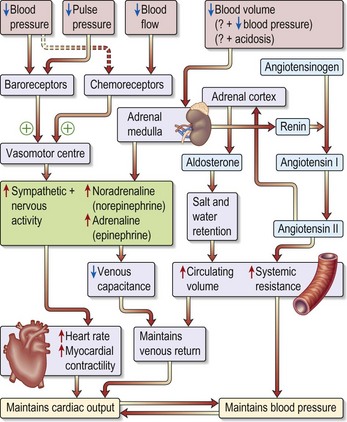
Physiology (Fig. 12.1)
Shock is ‘inadequate tissue oxygenation’ where there is failure of the circulatory system due to:
• Failure of the heart to maintain an adequate cardiac output, e.g. myocardial infarction
• Reduction in the volume of blood within the circulation, e.g. haemorrhage
• Loss of vascular tone within the circulatory system, e.g. septicaemia
Causes of shock
• Cardiogenic: myocardial infarction, tamponade, aortic dissection, pulmonary embolism
• Sepsis: infective causes, e.g. pneumonia, urinary tract infection or meningococcal septicaemia or ‘systemic inflammation’, resulting from trauma, post-surgery or anaphylaxis
Is the shock state in Case 1 due to myocardial infarction, an obstructed circulation or other shock-inducing factors?
Clinical examination
In assessing the shocked patient the following indices should be monitored:
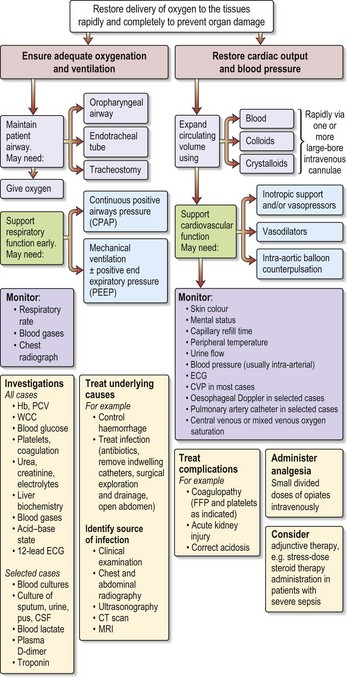
Other investigations (see Fig 12.2)
• Arterial blood gas analysis: in hypovolaemic shock (as in all shock states) there is a metabolic acidosis with a high hydrogen ion concentration and low bicarbonate concentration. In cases with respiratory complications the pO2 and pCO2 values will help indicate the need for ventilatory support.
• Lactate levels: blood lactate levels rise approximately in proportion to the severity of the shock.
• X-rays: these are usually of little value in the acute stages of shock management. A CXR will exclude any treatable pathology, such as a pneumothorax or haemothorax often complicating insertion of monitoring lines. A CT scan may be helpful in, for example, a case of trauma.
How would you treat?
Case 1
Progress.
Information
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree