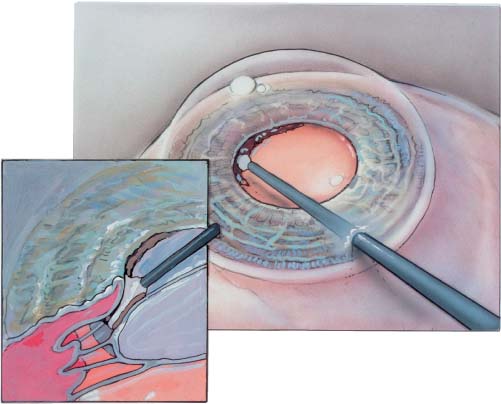
Chapter 6 The meiotic pupil is a relatively common problem. It is defined by Howard Fine1 as a pupil smaller than 4 mm. Gimbel reported an incidence of 1.6% patients with small pupils out of 1880 consecutive phaco surgeries.2 The presence of a small pupil has been established as a significant risk factor for the development of complications during cataract surgery. Therefore, the surgeon is compelled to acquire skills to effectively manage a small pupil. A small pupil makes visualization of the anterior chamber difficult and diminishes depth perception while working deep to the iris. It can make all the significant steps of phacoemulsification difficult, including capsulorrhexis, hydro-steps, phaco, irrigation and aspiration (I&A), and intraocular lens (IOL) insertion. There are many causes of a small pupil. The most common is pseudoexfoliation.3 These patients have fibrotic pupillary sphincters as well as weak capsules and friable zonules.4 Patients with anterior uveitis may have posterior synechiae. Previous trauma with iris scarring or posterior synechiae may cause a small pupil. The incidence of combined cataract and glaucoma increases with age; many of these patients will be on long-term mitotic drops with secondary pupillary fibroses and extremely small pupils. Finally, some older patients just don’t dilate well. The primary goal of managing the meiotic pupil is to achieve an adequate pupillary aperture to perform safe phacoemulsification. This size will vary with the experience of each surgeon. In addition, there is an important secondary goal of pupil management—the maintenance of both pupillary function and cosmetic appearance after pupillary dilation (Tables 6–1 and 6–2). If possible, discontinue the use of miotic agents such as pilocarpine at least 2 weeks prior to surgery. On the day of surgery one protocol is the following: 1% cyclopentolate hydrochloride (Cyclogyl) 1% tropicamide (Mydriacyl) 2.5% phenylephrine (Neo-Synephrine) Topical nonsteroidal antiinflammatory drugs(NSAIDs) such as ketorolac tromethamine 0.5% (Acular) Each is given every 5 to 15 minutes for four times prior to surgery. If the pupil does not dilate well, add one drop of phenylephrine (Neo-Synephrine) 10% viscous. It is inadvisable to use aqueous phenylephrine in this concentration, as intractible cardiac arrhythmias have been associated with systemic absorption of the liquid form. Topical anesthesia can be performed even in cases with small pupils. However, the following can also be performed with retro/peribulbar anesthesia. With topical anesthesia, after creation of the paracentesis, 0.2 to 0.4 cc of 1% unpreserved lidocaine is injected into the anterior chamber. It is then deepened with viscoelastic. Usually a 3.0-mm clear corneal incision 1.75 to 2.00 mm into clear cornea is established. If indicated, a Kuglen hook is then used to examine the iris for adhesions and mobility. Peripupillary adhesions can often be broken at this time. Additionally, both the blunt viscoelastic cannula as well as gentle viscodissection can be used to sweep under the iris to release posterior synechiae (Fig. 6–1).
IRIS PROBLEMS
MANAGEMENT OF A SMALL PUPIL DURING CATARACT SURGERY
ETIOLOGY
PREOPERATIVE MANAGEMENT
SURGICAL TECHNIQUE—LYSIS OF SYNECHIAE
1. Make a clinic note regarding dilation status so that preoperatively you know what to expect from pharmacologic dilation 2. Add a nonsteroidal antiinflammatory drug (NSAID) and phenylephrine 10% viscous if a patient dilates poorly 3. A retrobulbar block assists pharmacologic dilation 4. Always have a Beehler pupil dilator sterile and ready to use anytime the pupillary size appears too small 5. Always have one set of micro-iris hooks available 6. Use additional postoperative steroid, NSAID, and meiotics |
Occasionally, thin veneer-like membranes will remain on the anterior capsule. These should be removed with a Utrata (not sharp-tipped) or a Kelman McPherson forceps, as this will allow better control of the capsulorrhexis. If the pupil is large enough after these steps, no further manipulations are necessary. As all iris manipulation causes iris damage and subsequent breakdown of the blood–aqueous barrier, the less the iris is manipulated, the better.
1. Too much phenylephrine 10%, especially the aqueous form, may cause intractable cardiac arrhythmias 2. Do not operate in the presence of a small pupil; first make it larger 3. Disregard the increased iris fragility throughout the remainder of the case 4. Implantation of a 5.5-mm or smaller optic intraocular lens (IOL) |
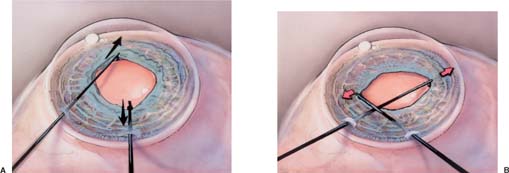
IRIS STRETCH—TWO INSTRUMENTS
Simple stretch techniques often work and usually eliminate the need of scissors or retractors. One simple method utilizes two instruments. After filling the anterior chamber (AC) with viscoelastic, and before creating the capsulorrhexis, two Kuglen hooks or Y hooks are employed. One is inserted through the incision and the other through the paracentesis. The instrument tips are moved toward the limbus employing a slow, constant bimanual stretch (Fig. 6–2A). A single stretch will often be adequate. However, to obtain maximum pupil size a second stretch 90 degrees away will usually create a significant increase in the pupil diameter1,5–7 (Fig. 6–2B). The chamber can then be re-deepened with viscoelastic, and surgery commenced.
FIGURE 6–1 During injection of visco-elastic, viscodissection of iris synechiae is accomplished by injecting viscoelastic between the iris and lens capsule prior to capsulorrhexis.
FIGURE 6–2 (A) Using two Kuglen hooks, the iris is stretched in the axis of the wound. (B) Next it is stretched in the opposite axis.
Histologically, it is observed that stretching causes micro–sphincter tears. Too rapid of a stretch may increase the length of these microtears, creating macrotears and permanent secondary mydriasis. Done slowly and gently, the end result is usually a round, functional pupil.
IRIS STRETCH—BEEHLER DILATOR
Moria Company (no. 18032), in association with Beehler, has come up with an instrument that produces a four-point stretch using one hand. It requires an incision of 3.0 mm or larger, and is reusable and extremely effective (Fig. 6–3). Due to its delicate nature and poor finish, it must be carefully cleaned of adherent viscoelastic after each use. It may then be sterilized and held available, prepackaged, for use at a moment’s notice. A three-point dilator, with a smaller diameter barrel and an angulation for small clear corneal incisions (2.5 mm), is also available. A similar but smaller two-point dilation instrument, the Keuch pupil dilator, is produced by Katena (K-3-4950).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree