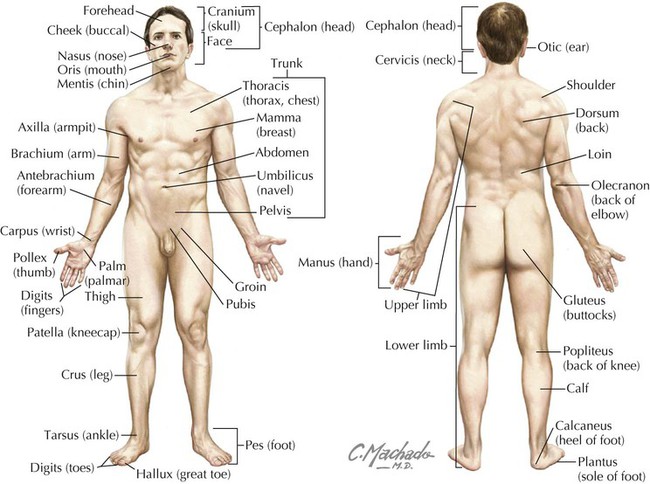
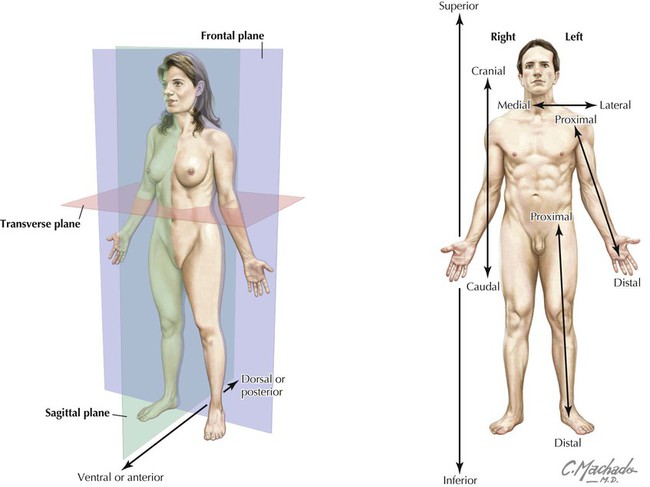
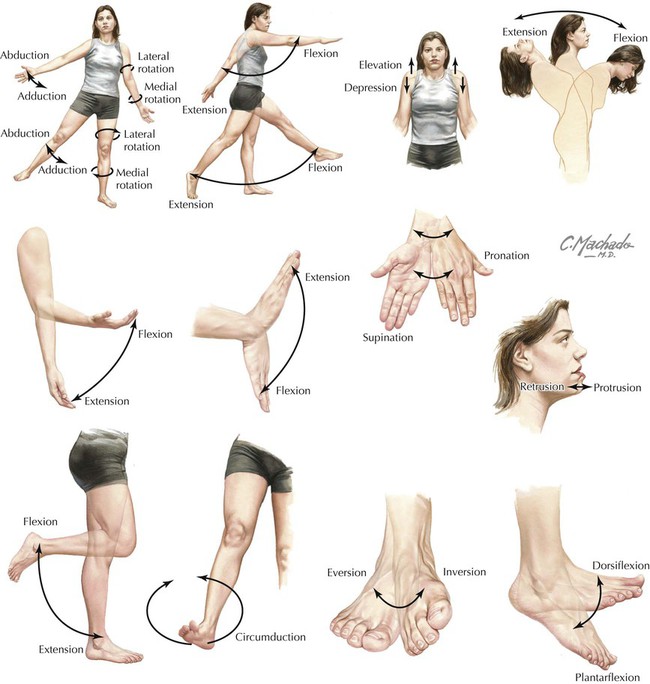
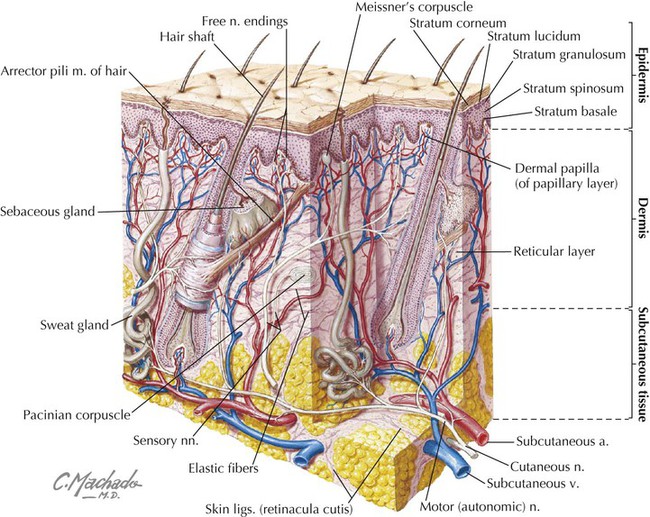
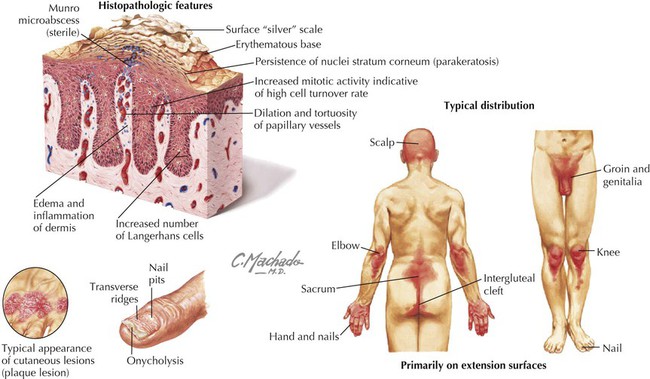
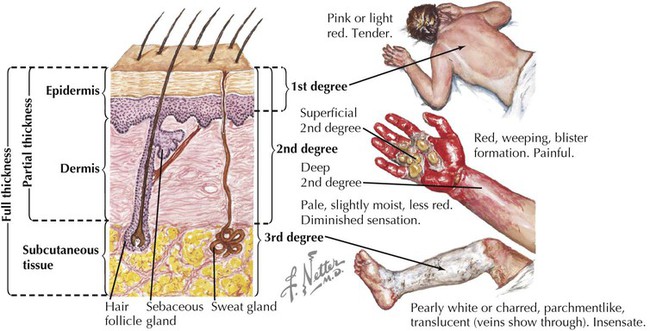
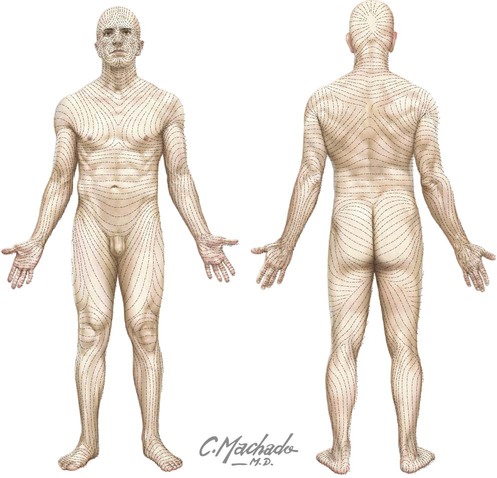
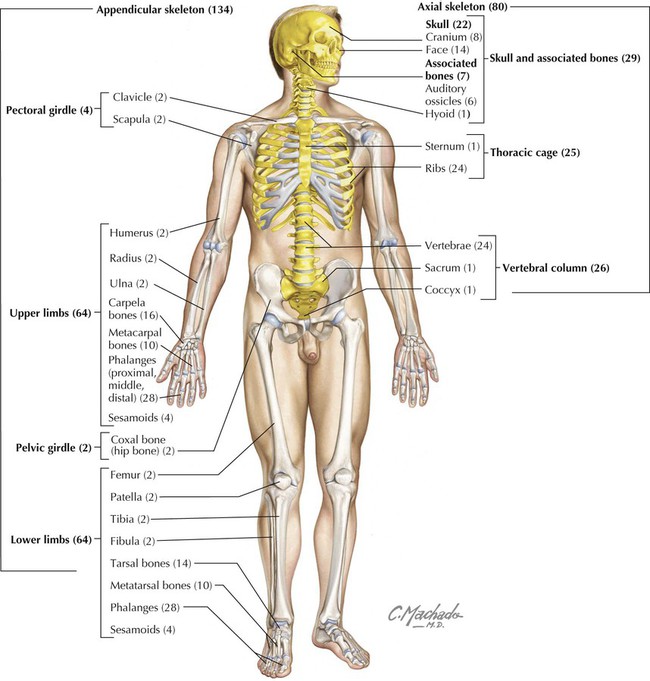
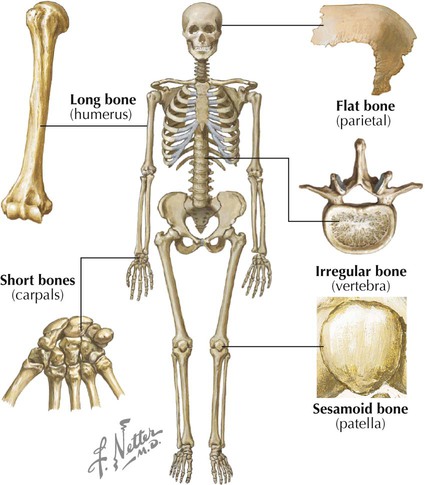
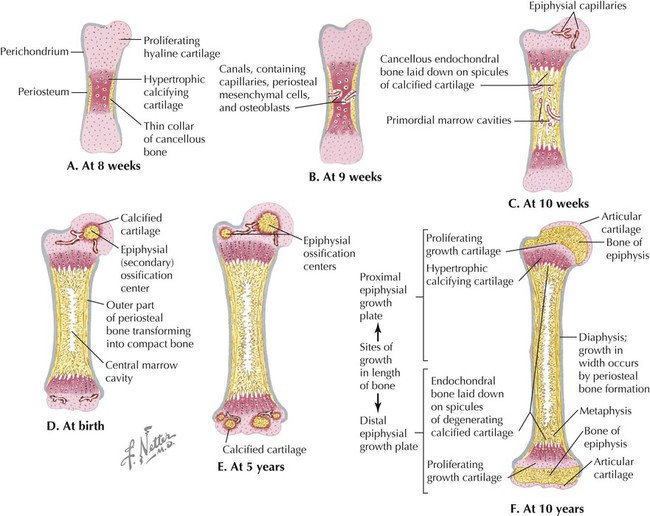
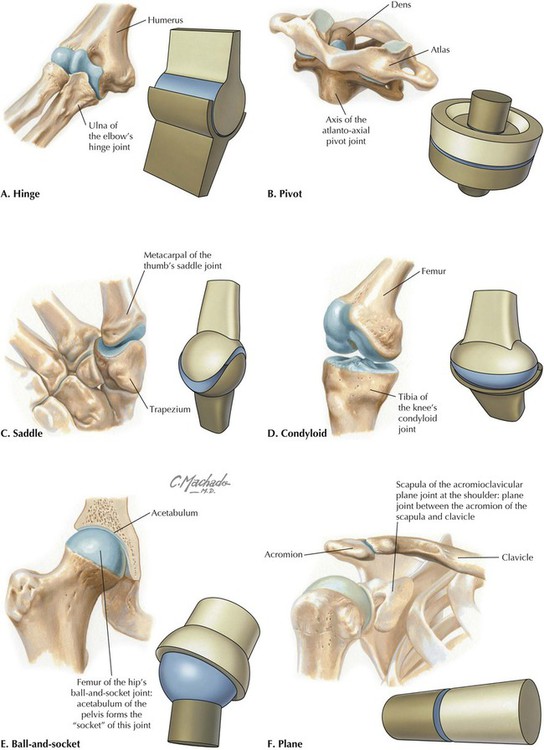
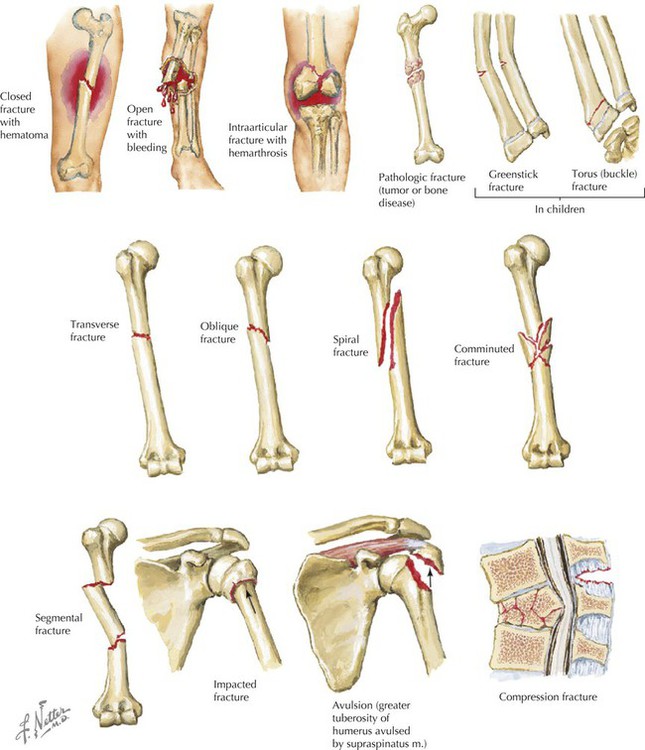
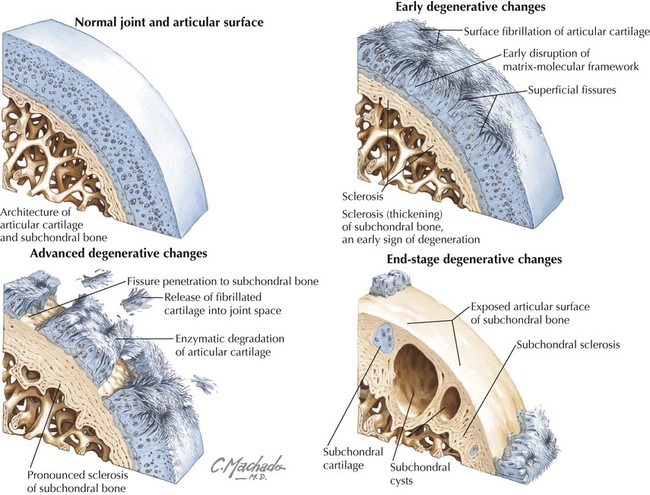
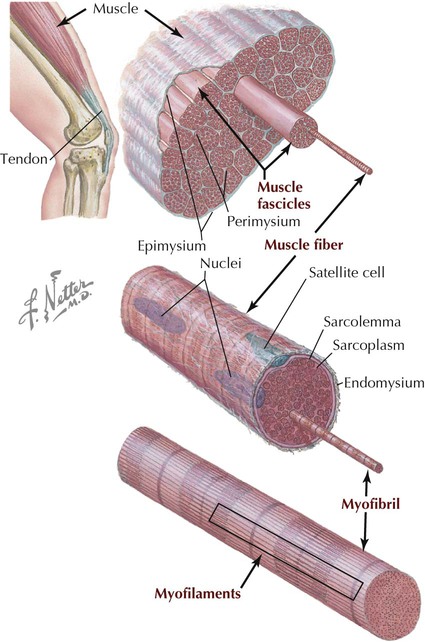
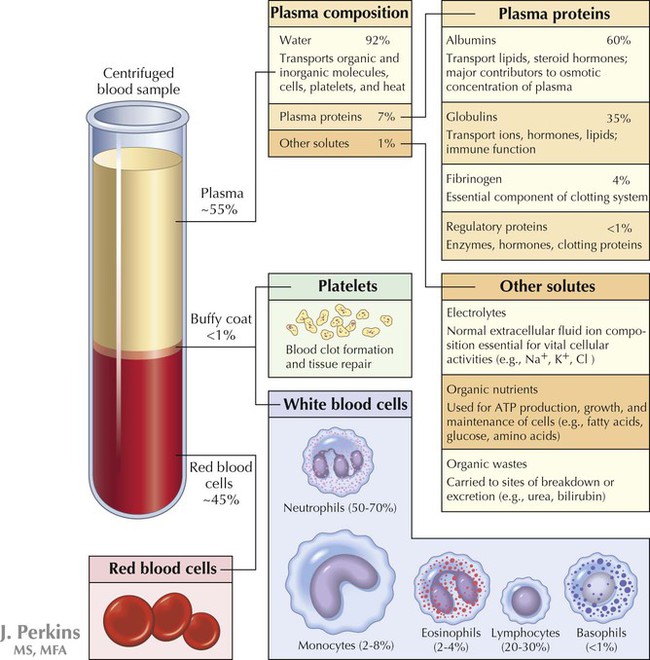
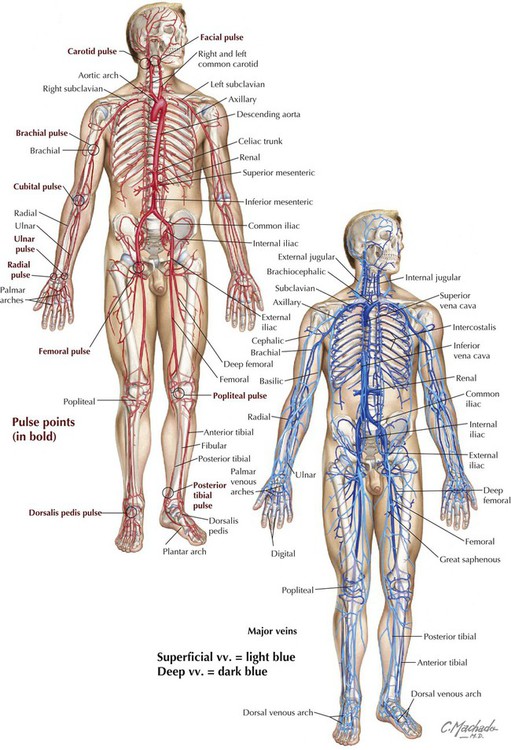
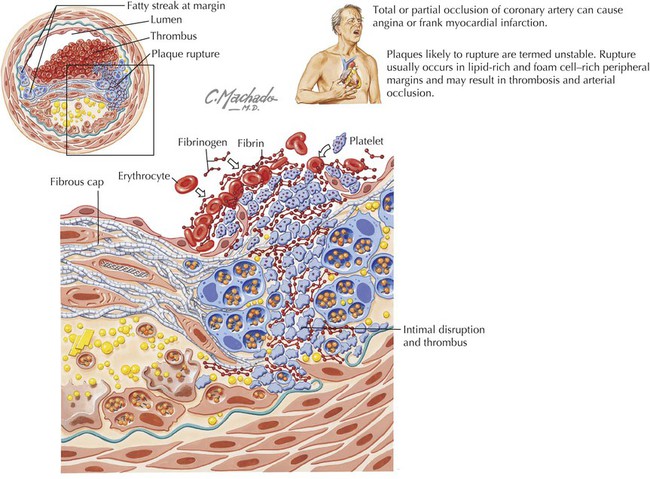
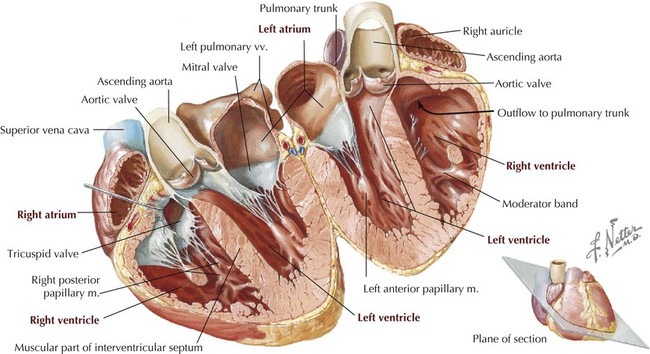
By convention, anatomical descriptions of the human body are based on a person in the anatomical position (Fig. 1-1), as follows: Anatomical descriptions often are referenced to one or more of three distinct body planes (Fig. 1-2 and Table 1-1), as follows: TABLE 1-1 General Terms of Anatomical Relationship • Sagittal plane: vertical plane that divides the body into equal right and left halves (median or midsagittal plane) or a plane parallel to the median sagittal plane (parasagittal) that divides the body into unequal right and left portions. • Frontal (coronal) plane: vertical plane that divides the body into anterior and posterior portions (equal or unequal); this plane is at right angles to the median sagittal plane. • Transverse (axial) plane: horizontal plane that divides the body into superior and inferior portions (equal or unequal) and is at right angles to both the median sagittal and the frontal planes (sometimes called cross sections). Key terms of relationship used in anatomy and the clinic are summarized in Table 1-1. A structure or feature closer to the front of the body is considered anterior (ventral), and one closer to the back is termed posterior (dorsal). The terms medial and lateral are used to distinguish a structure or feature in relationship to the midline; the nose is medial to the ear, and in anatomical position, the nose also is anterior to the ear. Sometimes these terms of relationship are used in combination (e.g., superomedial, meaning closer to the head and nearer the median sagittal plane). Body movements usually occur at the joints where two or more bones or cartilages articulate with one another. Muscles act on joints to accomplish these movements and may be described as follows: “The biceps muscle flexes the forearm at the elbow.” Figure 1-3 summarizes the terms of movement. • Bones: fine features of bones (processes, spines, articular surfaces) may be variable depending on the forces working on a bone. • Muscles: vary with size and fine details of their attachments (it is better to learn their actions and general attachments rather than focus on detailed exceptions). • Organs: the size and shape of some organs will vary depending on their normal physiology or pathophysiologic changes that have occurred previously. • Arteries: surprisingly consistent, although some variation is seen in the branching patterns, especially in the lower neck (subclavian branches) and in the pelvis (internal iliac branches). • Veins: consistent, although variations, especially in size and number of veins, can occur and often can be traced to their complex embryologic development; veins generally are more numerous than arteries, larger, and more variable. • Protection: against mechanical abrasion and in immune responses, as well as prevention of dehydration • Temperature regulation: largely through vasodilation, vasoconstriction, fat storage, or activation of sweat glands • Sensations: to touch by specialized mechanoreceptors such as pacinian and Meissner’s corpuscles; to pain by nociceptors; and to temperature by thermoreceptors • Endocrine regulation: by secretion of hormones, cytokines, and growth factors, and by synthesis and storage of vitamin D • Exocrine secretions: by secretion of sweat and oily sebum from sebaceous glands The skin consists of two layers (Fig. 1-4): • Epidermis: outer protective layer consisting of a keratinized stratified squamous epithelium derived from the embryonic ectoderm. • Dermis: dense connective tissue layer that gives skin most of its thickness and support, and is derived from the embryonic mesoderm. • First-degree: burn damage is limited to the superficial layers of the epidermis; termed a superficial burn, clinically it causes erythema. • Second-degree: burn damage includes all the epidermis and extends into the superficial dermis; termed a partial-thickness burn, it causes blisters but spares the hair follicles and sweat glands. • Third-degree: burn damage includes all the epidermis and dermis and may even involve the subcutaneous tissue and underlying deep fascia and muscle; termed a full-thickness burn, it causes charring. The human skeleton is divided into two descriptive regions (Fig. 1-5): • Axial skeleton: bones of the skull, vertebral column (spine), ribs, and sternum, which form the “axis” or central line of the body (80 bones). • Appendicular skeleton: bones of the limbs, including the pectoral and pelvic girdles, which attach the limbs to the body’s axis (134 bones). The skeleton is composed of a living, dynamic, rigid connective tissue that forms the bones and cartilages. Generally, humans have about 214 bones, although this number varies, particularly in the number of small sesamoid bones that may be present. (Many resources claim we have only 206 bones but have not counted the eight sesamoid bones of the hands and feet.) Cartilage is attached to some bones, especially where flexibility is important, or covers the surfaces of bones at points of articulation. About 99% of the body’s calcium is stored in bone, and many bones possess a central cavity that contains bone marrow—a collection of hemopoietic (blood-forming) cells. Most of the bones can be classified into one of the following five shapes (Fig. 1-6): The functions of the skeletal system include: There are two types of bone: • Compact: a relatively solid mass of bone, commonly seen as a superficial layer of bone, that provides strength. • Spongy (trabecular or cancellous): a less dense trabeculated network of bone spicules making up the substance of most bones and surrounding an inner marrow cavity. Long bones also are divided into the following descriptive regions (Fig. 1-7): • Epiphysis: the ends of long bones, which develop from secondary ossification centers. • Epiphysial plate: site of growth in length; contains cartilage in actively growing bones. • Metaphysis: site where the bone’s shaft joins the epiphysis and epiphysial plate. • Diaphysis: the shaft of a long bone, which represents the primary ossification center and the site where growth in width occurs. As a living, dynamic tissue, bone receives a rich blood supply from: • Nutrient arteries: usually one or several larger arteries that pass through the diaphysis and supply the compact and spongy bone, as well as the bone marrow. • Metaphysial and epiphysial arteries: usually from articular branches supplying the joint. • Periosteal arteries: numerous small arteries from adjacent vessels that supply the compact bone. • Condyle: rounded articular surface covered with articular (hyaline) cartilage • Crest: a ridge (narrow or wide) of bone • Epicondyle: prominent ridge or eminence superior to a condyle • Facet: flat, smooth articular surface, usually covered with articular (hyaline) cartilage • Fissure: very narrow “slitlike” opening in a bone • Foramen: round or oval “hole” in the bone for passage of another structure (nerve or vessel) • Fossa: a “cuplike” depression in the bone, usually for articulation with another bone • Groove: a furrow in the bone • Line: fine linear ridge of bone, but less prominent than a crest • Malleolus: a rounded eminence • Meatus: a passageway or canal in a bone • Process: bony prominence that may be sharp or blunt • Protuberance: protruding eminence on an otherwise smooth surface • Ramus: thin part of a bone that joins a thicker process of the same bone • Spine: sharp process projecting from a bone • Trochanter: large, blunt process for muscle tendon or ligament attachment • Tubercle: small, elevated process • Tuberosity: large, rounded eminence that may be coarse or rough Bones develop in one of the following two ways: • Intramembranous formation: most flat bones develop in this way by direct calcium deposition into a mesenchymal (primitive mesoderm) precursor or model of the bone. • Endochondral formation: most long and irregularly shaped bones develop by calcium deposition into a cartilaginous model of the bone that provides a scaffold for the future bone. The following sequence of events defines endochondral bone formation (Fig. 1-7, A-F): • Formation of a thin collar of bone around a hyaline cartilage model • Cavitation of the primary ossification center and invasion of vessels, nerves, lymphatics, red marrow elements, and osteoblasts • Formation of spongy (cancellous) endochondral bone on calcified spicules • Diaphysis elongation, formation of the central marrow cavity, and appearance of the secondary ossification centers in the epiphyses • Long bone growth during childhood • Epiphysial fusion occurring from puberty into maturity (early to mid-20s) Joints are the sites of union or articulation of two or more bones or cartilages and are classified into one of the following three types (Fig. 1-8): • Fibrous (synarthroses): bones joined by fibrous connective tissue. • Cartilaginous (amphiarthroses): bones joined by cartilage, or by cartilage and fibrous tissue. • Synovial (diarthroses): bones joined by a joint cavity filled with a small amount of synovial fluid and surrounded by a capsule; the bony articular surfaces are covered with hyaline cartilage. Synovial joints generally allow for considerable movement and are classified according to their shape and the type of movement that they permit (uni-, bi-, or multiaxial movement) (Fig. 1-9), as follows: • Hinge (ginglymus): uniaxial joints for flexion and extension • Pivot (trochoid): uniaxial joints for rotation • Saddle: biaxial joints for flexion, extension, abduction, adduction, and circumduction • Condyloid (ellipsoid; sometimes classified separately): biaxial joints for flexion, extension, abduction, adduction, and circumduction • Plane (gliding): joints that only allow simple gliding movements • Ball-and-socket (spheroid): multiaxial joints for flexion, extension, abduction, adduction, mediolateral rotation, and circumduction • Skeletal: striated muscle fibers that are attached to bone and are responsible for movements of the skeleton (sometimes simplistically referred to as voluntary muscle) • Cardiac: striated muscle fibers that make up the walls of the heart and proximal portions of the great vessels • Smooth: nonstriated muscle fibers that line various organs, attach to hair follicles, and line the walls of most blood vessels (sometimes simplistically referred to as involuntary muscle) Skeletal muscle is divided into fascicles (bundles), which are composed of muscle fibers (muscle cells) (Fig. 1-10). The muscle fiber cells contain longitudinally oriented myofibrils that run the full length of the cell. Each myofibril is composed of many myofilaments, which are composed of individual myosin (thick filaments) and actin (thin filaments) that slide over one another during muscle contraction. • Flat: has parallel fibers, usually in a broad flat sheet with a broad tendon of attachment called an aponeurosis. • Quadrate: has a four-sided appearance. • Circular: forms sphincters that close off tubes or openings. • Fusiform: has a wide center and tapered ends. • Pennate: has a feathered appearance (uni-, bi-, or multipennate forms). Muscle contraction shortens the muscle. Generally, skeletal muscle contracts in one of three ways: • Reflexive: involuntary or automatic contraction; seen in the diaphragm during respiration or in the reflex contraction elicited by tapping a muscle’s tendon with a reflex hammer. • Tonic: maintains “muscle tone,” a slight contraction that may not cause movement but allows the muscle to maintain firmness necessary for stability of a joint and important in maintaining posture. • Phasic: two types of contraction; isometric contraction, where no movement occurs but the muscle maintains tension to hold a position (stronger than tonic contraction), and isotonic contraction, where the muscle shortens to produce movement. Muscle contraction that produces movements can act in several ways, depending on the conditions: • Agonist: the main muscle responsible for a specific movement (the “prime mover”). • Antagonist: the muscle that opposes the action of the agonist; as an agonist muscle contracts, the antagonistic muscle relaxes. • Fixator: one or more muscles that steady the proximal part of a limb when a more distal part is being moved. • Synergist: complements (works synergistically with) the contraction of the agonist, either by assisting with the movement generated by the agonist or by reducing unnecessary movements that would occur as the agonist contracts. The cardiovascular system consists of (1) the heart, which pumps blood into the pulmonary circulation for gas exchange and into the systemic circulation to supply the body tissues; and (2) the vessels that carry the blood, including the arteries, arterioles, capillaries, venules, and veins. The blood passing through the cardiovascular system consists of the following formed elements (Fig. 1-11): • Transport of dissolved gases, nutrients, metabolic waste products, and hormones to and from tissues • Prevention of fluid loss via clotting mechanisms • Regulation of pH and electrolyte balance • Thermoregulation through blood vessel constriction and dilation Blood circulates through the blood vessels (Fig. 1-12). Arteries carry blood away from the heart, and veins carry blood back to the heart. Arteries generally have more smooth muscle in their walls than veins and are responsible for most of the vascular resistance, especially the small muscular arteries and arterioles. Alternatively, at any point in time, most of the blood resides in the veins (about 64%) and is returned to the right side of the heart; thus veins are the capacitance vessels, capable of holding most of the blood, and are more variable and numerous than their corresponding arteries. The major arteries are illustrated in Figure 1-13. At certain points along the pathway of the systemic arterial circulation, large and medium-sized arteries lie near the body’s surface and can be used to take a pulse by compressing the artery against a hard underlying structure (usually a bone). The most distal pulse from the heart is usually taken over the dorsalis pedis artery on the dorsum of the foot. The major veins are also illustrated in Figure 1-13. Veins are capacitance vessels because they are distensible and numerous and can serve as reservoirs for the blood. Because veins carry blood at low pressure and often against gravity, larger veins of the limbs and lower neck region have numerous valves that aid in venous return to the heart (several other veins throughout the body may also contain valves). Both the presence of valves and the contractions of adjacent skeletal muscles help to “pump” the venous blood against gravity and toward the heart. In most of the body, the veins occur as a superficial set of veins in the subcutaneous tissue that connects with a deeper set of veins that parallel the arteries. Types of veins include: • Venules: very small veins that collect blood from the capillary beds • Veins: small, medium, and large veins that contain some smooth muscle in their walls, but not as much as their corresponding arteries • Portal venous systems: veins that transport blood between two capillary beds (e.g., the hepatic portal system) The heart is a hollow muscular (cardiac muscle) organ that is divided into four chambers (Fig. 1-14): • Right atrium: receives the blood from the systemic circulation via the superior and inferior venae cavae. • Right ventricle: receives the blood from the right atrium and pumps it into the pulmonary circulation via the pulmonary trunk and pulmonary arteries. • Left atrium: receives the blood from the lungs via pulmonary veins. • Left ventricle: receives the blood from the left atrium and pumps it into the systemic circulation via the aorta. • Protect the body against infection by activating defense mechanisms of the immune system. • Collect tissue fluids, solutes, hormones, and plasma proteins and return them to the circulatory system (bloodstream). Components of the lymphatic system include the following: • Lymph: watery fluid that resembles plasma but contains fewer proteins and may contain fat, together with cells (mainly lymphocytes and a few RBCs). • Lymphocytes: the cellular components of lymph, including T cells and B cells. • Lymph vessels: extensive network of vessels and capillaries in the peripheral tissues that transport lymph and lymphocytes. • Lymphoid organs: collections of lymphoid tissue, including lymph nodes, aggregates of lymphoid tissue along the respiratory and gastrointestinal passageways, tonsils, thymus, spleen, and bone marrow.
Introduction to the Human Body
1 Terminology
Anatomical Position
Terms of Relationship and Body Planes
TERM
DEFINITION
Anterior (ventral)
Near the front
Posterior (dorsal)
Near the back
Superior (cranial)
Upward, or near the head
Inferior (caudal)
Downward, or near the feet
Medial
Toward the midline or median plane
Lateral
Farther from the midline or median plane
Proximal
Near a reference point
Distal
Away from a reference point
Superficial
Closer to the surface
Deep
Farther from the surface
Median plane
Divides body into equal right and left parts
Midsagittal plane
Median plane
Sagittal plane
Divides body into unequal right and left parts
Frontal (coronal) plane
Divides body into equal or unequal anterior and posterior parts
Transverse plane
Divides body into equal or unequal superior and inferior parts (cross sections)
Movements
Anatomical Variability
2 Skin
3 Skeletal System
Descriptive Regions
Shapes and Function of Bones
Markings on the Bones
Bone Development
Types of Joints
4 Muscular System
5 Cardiovascular System
Blood Vessels
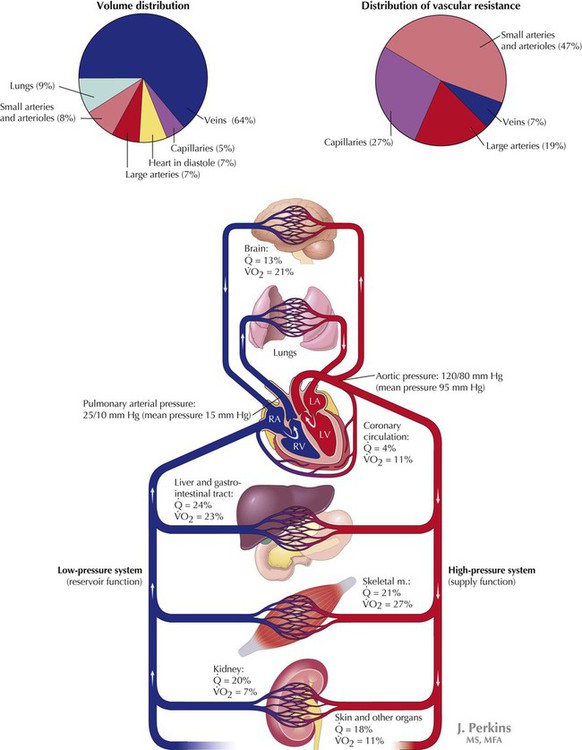
The amount of blood flow per minute ( ), as a percent of the cardiac output, and the relative percent of oxygen used per minute (
), as a percent of the cardiac output, and the relative percent of oxygen used per minute ( ) by the various organ systems are noted.
) by the various organ systems are noted.
Heart
6 Lymphatic System
General Organization
Introduction to the Human Body