Introduction to Impediments to Urine Flow
Sanjay Jain, MD, PhD
TERMINOLOGY
Definitions
Impediment to urine flow: Retrograde or hindered urine flow due to obstructive or nonobstructive causes
Reflux: Retrograde urine flow from bladder into ureters or kidney due to functional or physical defects of lower tract
Hydronephrosis: Dilatation of renal pelvis due to functional or physical impediment of urine flow
Obstructive nephropathy: Damage to kidney due to obstruction
Reflux nephropathy: Damage to kidney due to urine reflux
CLASSIFICATION
Type of Impediment
Obstructive
Physical
Internal urinary system obstruction: Stones, tumors of urinary tract, infections
External compression of urinary system: Tumors, pregnancy, retroperitoneal fibrosis, endometriosis, crossing vessels
Functional
Ureter or collecting duct dysfunction
Congenital
Ureteropelvic junction obstruction (UPJO)
Primary obstructive megaureter or ureterovesical junction obstruction (UVJO)
Ureterocele
Posterior urethral valves (PUV)
Acquired
Nonobstructive: Vesicoureteral reflux (VUR)
Primary VUR
Secondary VUR
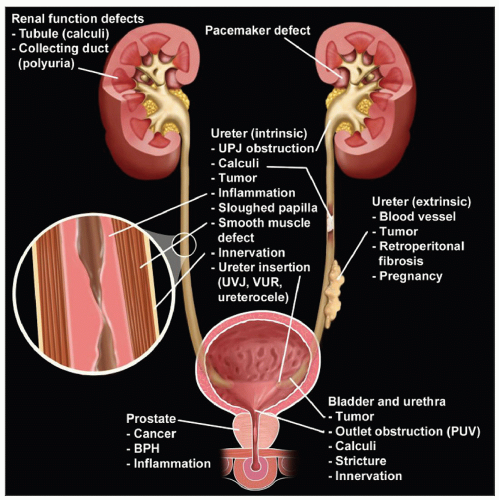
Region of Impediment and Associated Major Abnormalities
Upper urinary tract
Kidney (tubules, collecting duct)
UPJO
Lower urinary tract
Ureter
UPJO
UVJO or megaureter
Ureterocele
Bladder and ureter
VUR
Bladder and urethra
PUV
ETIOLOGY/PATHOGENESIS
Developmental Mechanisms
UPJO
Most common cause of obstructive nephropathy
Kidney
Abnormal water absorption or collecting duct cell function (functional obstruction)
Abnormal pacemaker function regulating peristalsis (functional obstruction)
Ureter
Abnormal ureter or pelvic wall development (increased extracellular matrix, disorganized smooth muscle) leading to defective peristalsis (functional obstruction)
Extrinsic
Crossing by lower pole renal vessels (physical obstruction)
Nervous system (pyeloureteral innervation) mediated defects in peristalsis (functional obstruction)
Megaureter
UVJO, abnormal muscular development or stricture, ureter insertion into bladder may be normal
Supernumerary ureters ectopically inserted into bladder
Refluxing megaureter due to primary or secondary reflux
Ureterocele
Distal blind-ending ureter often in completely duplicated collecting system
Primary VUR
Distal Wolffian duct (WD) &/or ureter maturation
Abnormal ureteric bud (UB) budding site
Failure of ureter insertion into bladder, abnormality of vesicoureteral junction
Failure of ureter to separate from WD
Abnormal common nephric duct (CND) degeneration
Most common congenital anomalies of kidney and urinary tract (CAKUT)
50% of children with UTIs may have VUR
15-34% of children with asymptomatic bacteriuria may have VUR
PUV
Failure of urogenital membrane disintegration
Genetic Mechanisms
UPJO
Families exhibiting autosomal dominant inheritance have been reported; cannot rule out other modes of inheritance
Genes associated or mutated
Shh, Bmp4, Tshz3, Adamts1, Dlgh1, Calcineurin, renin-angiotensin system (RAS), Tbx18, Id2, Limp2
Primary VUR
Genetically heterogeneous
Inheritance patterns include autosomal dominant, autosomal recessive, polygenic, sporadic, recessive X-linked with incomplete penetrance and variable expressivity
Not unusual to skip generations
Individuals in same family may have VUR or other CAKUT
Modifier genes or epigenetics can affect phenotype
80% chance in monozygotic twin
32% in siblings
Known genetic mutations account for only small number of cases
Genome-wide association studies (GWAS) identified several common variants of primary VUR; however, in most cases it is unknown if the associated genes are causal
Long-range effects of common variants
Rare deleterious variant burden in coding, splice junctions, or insertions/deletions may underlie genetic causes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree