OVERVIEW
- Medically unexplained symptoms (MUS) are characterised by disturbances of function—including physiological, neurological and cognitive processes
- Using what is currently known about disturbed function, it is possible to develop coherent and plausible models of conditions in order to explain what is going on to patients
- Sharing explanations and understanding concerns allows the doctor and patient to work together. Describing symptoms as disorders of function is an acceptable way of doing this
Aim
This book aims to help general practitioners (GPs) and other generalists to understand and treat conditions associated with symptoms that appear not to be caused by physical disease. This lack of explanation due to visible pathology means they are often called medically unexplained symptoms (MUS). This book takes the view that MUS are disorders of function, rather than structure, and so the book will refer to them as functional symptoms. Although we do not fully understand the nature of the disturbed function, research is making this clearer and several mechanisms, including physiological, neurological and cognitive processes play a part in symptoms. This book also takes the view that by using what is currently known about functional symptoms, it is possible to develop coherent and plausible models to explain what is going on. This book aims to help doctors explain the medically unexplained—both to themselves and to their patients.
Symptoms that appear not to be caused by physical disease are a challenge to doctors and patients. Both have to simultaneously consider the possibility of serious illness (either physical or mental) while seeking to contain and reduce the symptoms and the threat they represent. This is not easy. In order to deal with MUS, and the patients who present with them, doctors need to apply a range of clinical skills: from empathic history taking and focused examination, through careful assessment of probabilities, to communication, explanation and—sometimes—support. This book assumes you already have those skills to some extent; it aims to show ways of using, and developing, them in order to deal with these common problems.
An approach to MUS
The ABC of Medically Unexplained Symptoms is not a book about the somatisation of mental distress from a psychoanalytic perspective. It does not take the view that unexplained symptoms are a way of communicating need in people who cannot otherwise do so. Rather it takes a mechanistic view of symptoms as the result of interacting processes—some physiological, some neuropsychological—that lead to persistent unpleasant feelings and distress. This approach is similar to that used in pain medicine, with which it has much in common; indeed many unexplained symptoms and syndromes include pain.
This introductory chapter addresses three questions: what do we mean by medically unexplained symptoms; what causes medically unexplained symptoms; and what should we call medically unexplained symptoms?
What do we mean by medically unexplained symptoms?
The simple answer to this question is ‘physical symptoms that cannot be explained by disease’, but it has several problems. First, this book is written largely from a primary care perspective and although it may be that every possible disease has been ruled out in tertiary care, this is not often the case in primary care. Furthermore, not all ‘diseases’ have consistent pathology—migraine is an excellent example of a syndrome that we have kept on the ‘explained’ side of the dividing line between explained and medically unexplained symptoms but where the problem is one of disturbed function rather than structure. Even persistent back pain, which initially seems an obvious ‘explained’ symptom, shows almost no correlation between symptom severity and structural abnormality.
Instead of this simple ‘absence of disease’ answer, it can be helpful to think of three different meanings: symptoms with low probability of disease; functional somatic syndromes; and experiencing multiple physical symptoms. This book will use the adjective ‘functional’ in relation to symptoms or syndromes (i.e. MUS) to mean simply that we can best understand them in terms of disturbed function without altered structure. In general it will use the term ‘organic’ to refer to conditions associated with pathological change.
Symptoms with low probability of disease
This term has recently been introduced in an attempt to capture the uncertainty that is inherent in this field. Around 10% of patients in primary care with persistent so-called MUS eventually turn out to have an alternative diagnosis. The proportion is rather lower in some forms of secondary care but nonetheless all doctors will have seen a patient whom they originally thought had a functional symptom but turned out to have a disease. We believe that the concept of symptoms with low probability of disease is useful though, as it can be applied to a patient with positive pointers to a functional disorder and with no red flags for serious illness to indicate a ‘working diagnosis’. Chapters 3 and 4 describe the recognition of physical illness and emotional disorders in patients with MUS.
Functional somatic syndromes
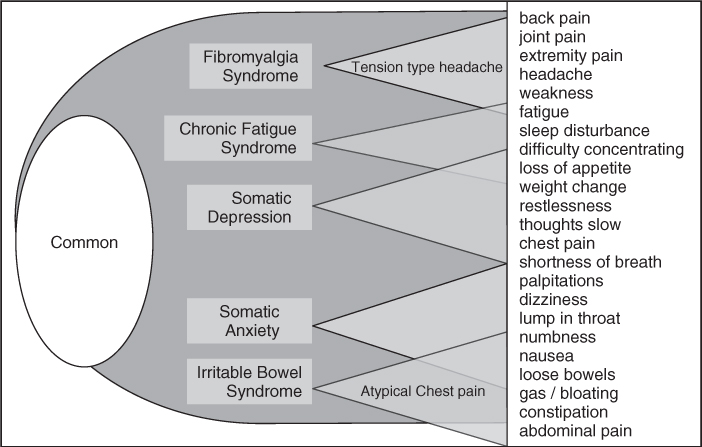
The common functional physical symptoms—fatigue, headache, light-headedness, headache, palpitations, chest pain, nausea, bloating, abdominal pain, musculoskeletal pain and weakness often occur together. Some of these clusters—particularly when they present to a given clinical specialty—are commonly grouped together as a syndrome. So gastroenterology has the irritable bowel syndrome (IBS), rheumatology has chronic widespread pain and fibromyalgia, and gynaecologists have chronic pelvic pain. As Figure 1.1 shows, and as described further in Chapter 2, all these symptoms overlap; to the extent that some experts argue that all the syndromes represent facets of a single disorder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree