Chapter 1
Introducing Multimorbidity
Martin Fortin1, Stewart W. Mercer2, and Chris Salisbury3
1Family Medicine Department, Université de Sherbrooke, Centre de Santé et de Services Sociaux de Chicoutimi, Canada
2General Practice and Primary Care, Institute of Health and Wellbeing, University of Glasgow, UK
3Centre for Academic Primary Care, NIHR School for Primary Care Research, School of Social and Community Medicine, University of Bristol, UK
Overview
- Multimorbidity refers to the presence of several co-occurring long-term conditions, being related or not, in a given patient
- Comorbidity refers to any additional condition that may occur during the clinical course of a patient who has an index condition that is the focus of interest
- Different terms such as frailty, disability and complexity are used by clinicians and researchers to describe conditions that are related to multimorbidity, representing different concepts
- Multimorbidity is not a medical diagnosis with well-defined criteria but represents nonetheless a major challenge for patients and clinicians, and is an emerging priority for healthcare systems.
Background
Improvements in public health and advances in the provision of health care have contributed to an increased life expectancy. People affected by medical conditions that previously led to premature death can now survive much longer. Therefore, as the population ages, an increasing number of people are now living with long-term medical conditions. Furthermore, it is now recognized that many people have multiple long-term conditions, a state which we refer to in this book as ‘multimorbidity’.
First, we need to consider some issues of terminology and definition. The concept of multimorbidity is quite easy to understand in general terms, but quite hard to define, with many people using the same term to mean different things. Furthermore, the concept of multimorbidity is related to, but distinct from, other related terms such as comorbidity, complexity and frailty. From a medical diagnostic perspective, the terms comorbidity and multimorbidity have sometimes been used interchangeably, which is misleading. This chapter introduces the concepts of comorbidity and multimorbidity and differentiates them from other related concepts frequently used by clinicians and researchers (see Figure 1.1).
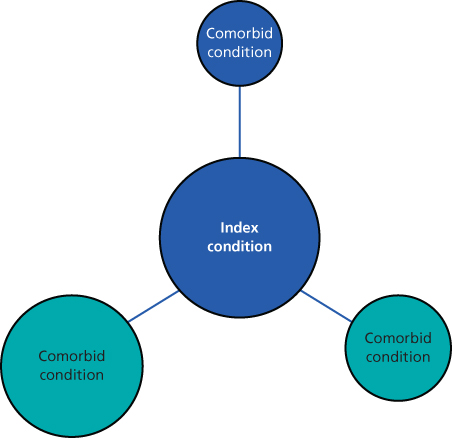
Figure 1.1 Conceptual diagram of comorbidity.
Adapted from: Boyd CM and Fortin M. 2011.
Box 1.1
What is the difference between multimorbidity and comorbidity?
How do the concepts of multimorbidity and frailty differ?
What are the two minimal components of a simple operational definition of multimorbidity?
Comorbidity
Feinstein, in his seminal paper published in 1970, is credited for recognizing that the therapeutic outcome of an index disease may vary depending on the type and nature of other accompanying disorders. He coined the term comorbidity: ‘any distinct additional clinical entity that has existed or that may occur during the clinical course of a patient who has the index disease under study’. In the 1980s and 1990s, some authors (mostly Germans publishing articles in English) started using the word multimorbidity when referring to patients with multiple simultaneous conditions without considering any one as the index condition. The existence of other equivalent terms for multiple concurrent conditions in the medical literature (Table 1.1) has led to ambiguity and inconsistency in their use.
Table 1.1 Terms used to designate multiple conditions.
| Comorbidity |
| Multimorbidity |
| Multi-morbidity |
| Polymorbidity |
| Poly-morbidity |
| Polymorbidities |
| Polypathology |
| Poly-pathology |
| Polypathologies |
| Pluripathology |
| Multipathology |
| Multi-pathology |
| Multipathologies |
Multimorbidity
In 1996, van den Akker and colleagues addressed this conceptual confusion and proposed the use of two terms only: comorbidity, with the original meaning provided by Feinstein (Figure 1.1); and multimorbidity, for situations where no index condition is considered (Figures 1.1 and 1.2 represent conceptual diagrams for comorbidity and multimorbidity). Since then, many authors have adopted these terms. It should be noted that the concept of comorbidity is more relevant to specialized care within particular fields of expertise, whereas the concept of multimorbidity is more relevant to primary care and general practice settings where designating an index disease is rarely useful.
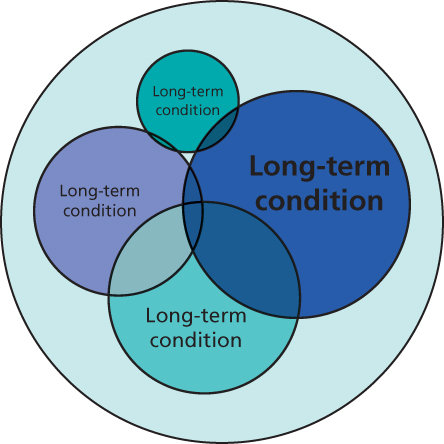
Figure 1.2 Conceptual diagram of multimorbidity.
Adapted from: Boyd CM and Fortin M. 2011.
Most (but not all) authors have used the term multimorbidity to mean patients with multiple long-term conditions, while others (most notably Barbara Starfield) have suggested that acute conditions should not be ignored. However, restricting the definition to long-term conditions is more useful for most purposes, because it the fact that conditions endure over a prolonged period that leads to the accumulation of problems in one individual. In the context of multimorbidity, the definition of a long-term or chronic condition is not straightforward. Time intervals of 3, 6 and 12 months have been used to define ‘long-term’ conditions. The World Health Organization has defined chronic condition as a health problem that requires ongoing management over a period of years or decades. At the very least, most people probably agree that a condition that lasts more than one year and requires ongoing medical care is a long-term condition. It is convenient at this point to specify that the term health condition is usually used in this context as it is more encompassing and less restrictive than terms such as disease (generally manifested by signs and symptoms) or illness (which also refers to a person’s perception of his or her health).
Other related concepts
Recognizing the presence of multimorbidity in a patient may lead to uncovering other challenging problems, not always well defined, but generally considered to be closely related to the presence of multiple diseases. These problems include concepts such as disability, frailty and patient complexity. Disability can be defined as a difficulty or dependency in carrying out activities that are essential for an independent living. Frailty represents a state of increased vulnerability to stressors that results from decreased physiologic reserves of multiple physiological systems, bearing a similarity with disability in associated outcomes. Patient complexity, although intuitively understood, is a multifaceted concept in which medical, social and behavioural factors play a role. All these concepts are more common in patients with multimorbidity and complicate the management of patients but are distinct from multimorbidity.
Other aspects related to the presence of multiple long-term conditions such as potential aetiological associations (where two conditions are caused by the same underlying factor), direct causation (where one condition causes a second condition) and correlation of associated risk factors with multimorbidity also has an impact on the management of patients.
Multimorbidity: clinical versus operational definition
Multimorbidity is not a medical diagnosis with well-defined criteria. It is rather a state by which the clinician along with the patient and/or the family faces the multiplicity of long-term conditions experienced by the patient. This represents the clinical definition of multimorbidity. In this respect and on clinical grounds, there is no clear number of conditions for which the patient is considered ‘multimorbid’. The cut-off may vary from one patient to another or between one clinician and another depending on many factors. Other states share the same imprecision, for example being old or frail. However, for the purposes of research and reporting, we need to agree on a definition that is measurable, comparable and conceptually sound. Various definitions are used in the literature, but many publications on multimorbidity lack clarity in the definition used.
A simple operational definition of multimorbidity includes at least two components: (1) the minimum number of conditions considered to be classified as ‘multimorbidity’ and (2) the conditions taken into account. In regard to the minimum number of conditions considered, the co-occurrence of two or more conditions is the operational definition most frequently used in the medical literature. However, cut-off counts of three, four and five long-term conditions have also been used or suggested by different authors. This distinction is important for reporting on the epidemiology of multimorbidity. But for clinical purposes, most doctors think of multimorbidity as referring to patients with multiple long-term conditions, without referring to a specific number.
The list of long-term conditions that have been taken into account in different studies on multimorbidity so far has varied greatly. Some authors have limited their investigation to a short list of conditions, ignoring all the other conditions a patient may have had. Others have included all possible long-term conditions experienced by the patient. This factor has an important impact on studies of the prevalence of multimorbidity (see Chapter 2). Not surprisingly, the longer the list of long-term conditions considered, the higher the probability of detecting the presence of multimorbidity. In reference to the type of conditions taken into account, the most prevalent chronic conditions with a high impact or burden on a given population should be included. Figure 1.3 presents a list of long-term conditions based on their frequency. From this we can imagine the impact of limiting the investigation to the top 5 or top 10 long-term conditions. For example, a patient with hypertension, renal failure, heart failure and osteoporosis would not be considered as a case of multimorbidity if we limit the investigation to the top 10! As a compromise to allow for good estimates in population prevalence studies, some authors have suggested the use of a minimal list of the 12 more frequent long-term conditions in a given context or setting. However, on clinical grounds and for a given patient, all long-term conditions should be considered.
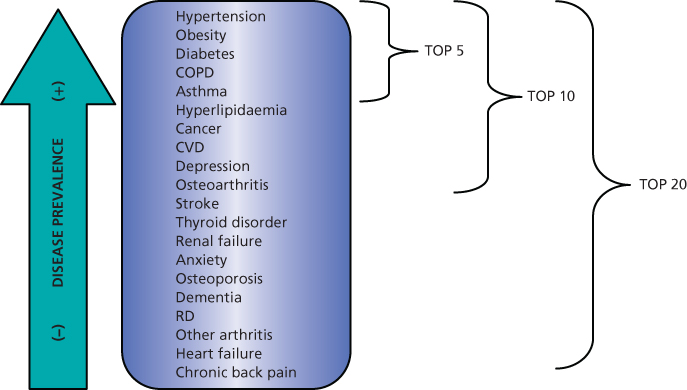
Figure 1.3 Diagram illustrating different cut-off points for the number of conditions taken into account: COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease and RD, rheumatic disease.
Clinical vignettes illustrating typical cases of multimorbidity in relationship with the other overlapping concepts of complexity and comorbidity are presented in Boxes 1.2–1.4.
Box 1.2 Multimorbidity
Mrs. MM, 48 years old
Mrs. MM is married and a mother of three teenagers. She works as a teacher in an elementary school. She is obese and being treated for hypertension and asthma, but her main concern is related to her recurrent depression for which she has been put on anti-depressant therapy for life. She does not exercise very often as she is symptomatic of a hip bursitis that has responded neither to medication nor to physical therapy. In the last 6 months, she has been bothered by symptoms of perimenopause with frequent hot flashes. She has been offered hormone therapy but she is uncertain about accepting as her mother died from breast cancer 2 years ago.
With at least six chronic conditions requiring management, Mrs. MM’s overall condition can be considered as multimorbidity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


