Intrapulmonary Synovial Sarcoma
Key Facts
Clinical Issues
Chest pain
Shortness of breath
Cough
Aggressive behavior with frequent recurrences and metastases
Macroscopic Features
Well-circumscribed, unencapsulated, solitary mass within lung parenchyma
Tan-white to gray, rubbery to gelatinous cut surface
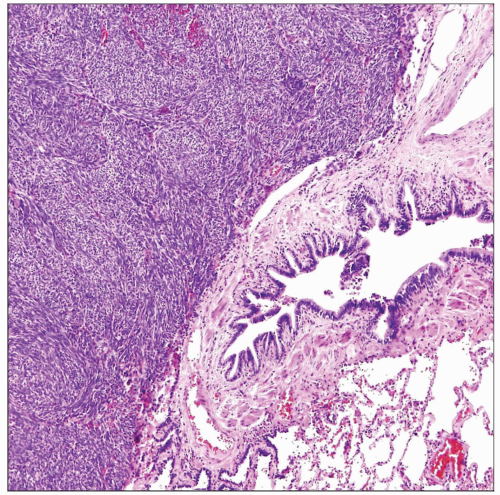
Microscopic Pathology
Fascicles of monotonous atypical spindle cells with variety of growth patterns
Herringbone pattern
Hemangiopericytic growth pattern
Storiform growth pattern
Neural-like palisading growth pattern
Tumor cells may display epithelioid morphology, with round nuclei surrounded by scant eosinophilic cytoplasm
Ancillary Tests
Tumor cells show focal (spotty) cytoplasmic positivity for cytokeratins (AE1/AE3, CAM5.2, CK8/18, CK19)
Tumor cells show focal (spotty) positivity for EMA
Tumor cells consistently show diffuse and strong positivity for Bcl-2 oncogene
Majority of cases (> 80%) show characteristic t(X;18) translocation
Fusion products include SYT/SSX1, SYT/SSX2, and SYT/SSX4
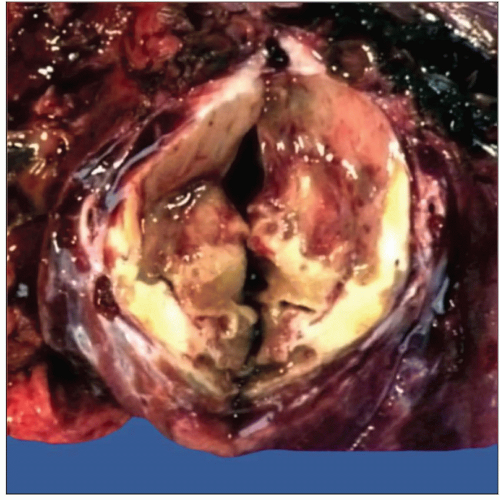 Gross appearance of primary synovial sarcoma of the lung shows well-circumscribed, intraparenchymatous tumor mass with areas of necrosis and glistening homogeneous gray-white cut surface. |
TERMINOLOGY
Definitions
Primary pulmonary malignant neoplasm characterized by a spindle cell morphology and displaying features of epithelial differentiation
CLINICAL ISSUES
Epidemiology
Incidence
Rare (< 1% of all lung neoplasms)
Age
Children to adults (mean age = 38 years)
Gender
Slight predilection for women
Presentation
Chest pain
Shortness of breath
Cough
Hemoptysis
May be asymptomatic and represent an incidental finding on chest x-ray
Treatment
Surgical approaches
Complete surgical excision is treatment of choice
Adjuvant therapy
Combination chemotherapy is indicated in advanced cases
Prognosis
Similar behavior as synovial sarcoma in peripheral soft tissue locations
Aggressive behavior with frequent recurrences and metastases
Metastases are to bone, central nervous system, liver, and skin
> 50% of patients die of tumor within 5-7 years after diagnosis
MACROSCOPIC FEATURES
General Features
Well-circumscribed, unencapsulated, solitary mass within lung parenchyma
Tan-white to gray, rubbery to gelatinous cut surface
Hemorrhage and necrosis
May show prominent cystic changes
Most often found in the periphery of the lung
Some tumors may be present endobronchially in central locations
Sections to Be Submitted
At least 1 section per centimeter of greatest tumor diameter
Size
1-20 cm (median size = 4 cm)
MICROSCOPIC PATHOLOGY
Histologic Features
Majority of tumors in the lung are of the monophasic spindle cell type
Fascicles of monotonous atypical spindle cells with variety of growth patterns
Herringbone pattern
Hemangiopericytic growth pattern
Storiform growth pattern
Neural-like palisading growth pattern
Some tumors may show prominent myxoid stromal changes
Areas of hemorrhage and necrosis
Foci of stromal hyalinization with bony metaplasia
Areas of vascular invasion
Cytologic Features
Monotonous population of atypical spindle cells with dense chromatin pattern and scant cytoplasm
Striking absence of intervening stroma supporting the tumor cells
Tumor cells may display epithelioid morphology, with round nuclei surrounded by scant eosinophilic cytoplasm
Variable mitotic activity (range = 2-20 mitoses per 10 high power fields)
ANCILLARY TESTS
Immunohistochemistry
Tumor cells show
Focal (spotty) cytoplasmic positivity for cytokeratins (AE1/AE3, CAM5.2, CK8/18, CK19)
Focal (spotty) positivity for EMA
Diffuse and strong positivity for Bcl-2
Positivity for CD99
May be positive for S100 protein, calponin, calretinin, HBME-1, and CD117