Intrapulmonary Solitary Fibrous Tumor
Key Facts
Clinical Issues
Cough
Chest pain
Dyspnea
Macroscopic Features
Generally well-circumscribed but unencapsulated intraparenchymatous masses
Rubbery, whorled, tan-white cut surface
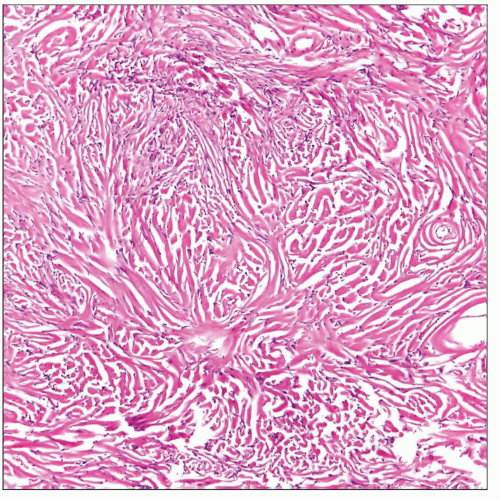
Microscopic Pathology
Variation of growth patterns, including fascicular, storiform, hemangiopericytic, herringbone, wavy neural, and angiofibromatous
Frequent admixture of cellular areas with hypocellular areas of stromal sclerosis
Rope-like linear pattern of stromal sclerosis is highly characteristic
Tumors may often entrap benign bronchial structures and airspaces at lesion periphery, simulating a biphasic neoplasm
Marked increase in cellularity and nuclear pleomorphism in cases undergoing malignant transformation
Increased mitotic activity (> 3 per 10 high power fields) in malignant cases
Ancillary Tests
Spindle cells are positive for CD34, Bcl-2, CD99, and vimentin
Negative for cytokeratins, EMA, S100 protein, muscle markers, and melanoma-associated markers
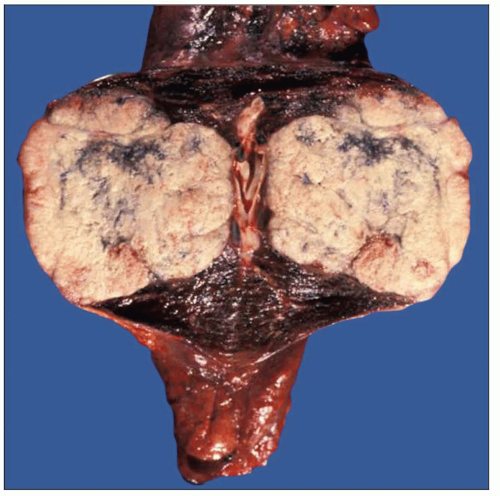 Gross appearance of an intrapulmonary solitary fibrous tumor shows a large, fleshy, bosselated tumor mass located within lung parenchyma expanding the pleura. |
TERMINOLOGY
Abbreviations
Solitary fibrous tumor (SFT)
Synonyms
Localized fibrous tumor, hemangiopericytoma, intrapulmonary fibroma, pulmonary fibrosarcoma
Definitions
Primary intrapulmonary neoplastic proliferation of dendritic fibroblasts
CLINICAL ISSUES
Presentation
Cough
Chest pain
Dyspnea
Clubbing of fingers
Treatment
Complete surgical excision (lobectomy) is favored approach
Prognosis
Majority of tumors (90%) are benign and cured by complete excision
About 10% behave aggressively (malignant solitary fibrous tumor) and can lead to death of patient
MACROSCOPIC FEATURES
General Features
Generally well-circumscribed but unencapsulated intraparenchymatous masses
Rubbery, whorled, tan-white cut surface
Can show areas of hemorrhage and necrosis (malignant cases)
MICROSCOPIC PATHOLOGY
Histologic Features
Benign SFT
Variation of growth patterns, including fascicular, storiform, hemangiopericytic, herringbone, wavy neural, and angiofibromatous
Frequent admixture of cellular areas with hypocellular areas of stromal sclerosis
Rope-like linear pattern of stromal sclerosis is highly characteristic
Tumors may often entrap benign bronchial structures and airspaces at lesion periphery, simulating a biphasic neoplasm
Usually sharp circumscription of the process from surrounding uninvolved lung parenchyma
High vascularity with numerous vessels of varying caliber size
Malignant SFT
Poor circumscription and foci of infiltration of lung parenchyma and bronchial structures
Marked increase in cellularity and nuclear pleomorphism
Increased mitotic activity (> 3 per 10 high-power fields)
Presence of frequent atypical mitoses
Multinucleated malignant giant cells
Foci of tumor cell necrosis
Foci of vascular invasion
Cytologic Features
Composed of small spindle cells without cytologic atypia in majority of cases
Spindle cells can show wavy nuclei simulating peripheral nerve sheath tumors
Cases with prominent stromal sclerosis can show small, round hyperchromatic nuclei devoid of cytoplasmic rims
Cases can be highly cellular with uniform cell population simulating growth pattern of synovial sarcoma
Malignant cases show atypical cells with enlarged nuclei, prominent nucleoli, and increased mitotic activity
Multinucleated cells of varying types may be observed in benign and malignant cases
Atypical, multinucleated giant cells are seen in malignant cases
Abnormal (bizarre, tripolar, “sunburst”) mitoses are seen in malignant cases
ANCILLARY TESTS
Immunohistochemistry
Spindle cells are positive for CD34, Bcl-2, CD99, and vimentin
Negative for cytokeratins, EMA, S100 protein, muscle markers, and melanoma-associated markers
Electron Microscopy
Transmission
Spindle cells show fibroblastic features ultrastructurally
Cells often show fine dendritic cytoplasmic processes that attach with neighboring cells
No evidence of smooth muscle, neural, myofibroblastic, melanocytic, or other type of cellular differentiation
DIFFERENTIAL DIAGNOSIS
Leiomyoma
Fascicles of spindle cells with fibrillary cytoplasm that appear to be cut at 90° angles
Tumor cells are positive for SMA, desmin, SMMS, and calponin, and negative for CD34, CD99, and Bcl-2
Synovial Sarcoma
Spindle cells are atypical with variable mitotic activity and very uniform appearance
Very scant vascularity and absence of stromal fibrosis
Tumor cells are positive for cytokeratins and EMA and negative for CD34
Characterized by distinctive cytogenetic translocation (X;18) in > 85% of cases
DIAGNOSTIC CHECKLIST
Clinically Relevant Pathologic Features
Histologic findings do not always correlate with prognosis
Some cases can metastasize and behave aggressively despite benign-appearing histologic features
Some cases with atypical morphologic features may behave in an indolent fashion
Pathologic Interpretation Pearls
Variation of histologic growth patterns (i.e., fascicular, herringbone, storiform, hemangiopericytic, etc.) is frequently observed
Alternating cellular and sclerotic areas are characteristic and often present
High vascularity with prominent vessels with patent lumens is always seen
Hemangiopericytic growth pattern is very common
“Hemangiopericytoma of lung” is synonymous with intrapulmonary solitary fibrous tumor
Increased cellularity, atypia, necrosis, and high mitotic activity are associated with aggressive or malignant behavior
SELECTED REFERENCES
1. Kouki HS et al: Solitary fibrous tumor of the lung. Gen Thorac Cardiovasc Surg. 56(5):249-51, 2008
2. Baliga M et al: Solitary fibrous tumor of the lung: a case report with a study of the aspiration biopsy, histopathology, immunohistochemistry, and autopsy findings. Diagn Cytopathol. 35(4):239-44, 2007
Image Gallery
Common Histologic Features
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree