
■ The C-arm fluoroscopy unit should be positioned to the patient’s right with the screen monitor clearly visible to the operating surgeon.
■ The bed should have a footboard placed and the patient should be well secured to the operating table, as reverse Trendelenburg position is required during the procedure.
Radiation Safety
■ The surgeon must be knowledgeable in the use of fluoroscopy. This should include successful completion of institutional training including certification for use of fluoroscopy in the operating theater.
■ All operating room personnel should don appropriate protective garments prior to scrubbing and gowning.
TECHNIQUES
CHOLANGIOCATHETER PLACEMENT
■ Cystic duct approach
■ The gallbladder infundibulum should be mobilized and dissection of Calot’s triangle should identify the cystic duct and artery entering the infundibulum.
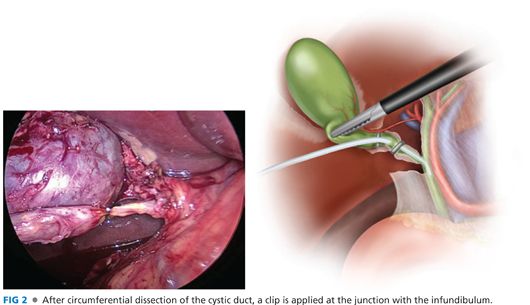
■ Once the cystic duct is circumferentially dissected, a clip should be placed across the cystic duct as proximal as possible to the infundibulum (FIG 2).
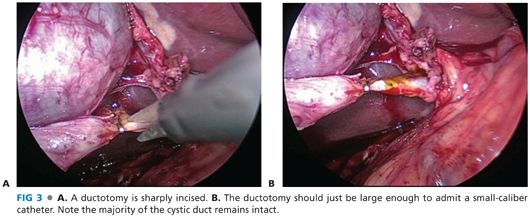
■ A ductotomy should be made along the cystic duct, leaving adequate length for subsequent double clip ligation. Care must be taken to avoid fully transecting the duct with this maneuver. An intact posterior-cephalad cystic duct wall is essential to maintain exposure and facilitate placement of the cholangiogram catheter (FIG 3). Note that it is typical for the ductotomy to enlarge with the necessary lateral retraction to provide exposure or with manipulation with the cholangiogram catheter. Furthermore, the skeletonized cystic duct typically lacks intrinsic strength and can tear easily with aggressive retraction once a ductotomy has been made.
■ Two techniques for placement of the cholangiocatheter for laparoscopic IOC have been described:
■ The first technique employs a 5-Fr cholangiocatheter inserted through an introducer sheath (FIG 4). This sheath, available as a component of commercially available cholangiogram catheter kits, is inserted through a separate incision along the right subcostal margin. Placement of this incision should be guided by location of the ductotomy. Ideally, the catheter enters the abdomen lateral and caudad to the cystic duct (FIG 5).

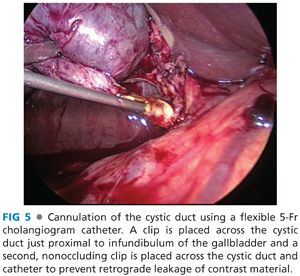
■ The catheter is then gently guided into the cystic duct with atraumatic technique and secured with a partially occluding clip placed just distal to the ductotomy.
■ An alternative technique is to use an Olsen-Reddick clamp (FIG 6). This device has a channel through the center of the clamp to accommodate a 5-Fr cholangiocatheter. The clamp is advanced though a laterally placed trocar. Once intraabdominal, the jaws of the clamp are opened and the cholangiocatheter is inserted through the center channel until the catheter tip extends beyond the jaws of the clamp. The catheter is then directed into the cystic duct. Once in place, the jaws of the clamp are closed around the cystic duct and cholangiocatheter, preventing leakage of contrast through the ductotomy (see FIG 2).
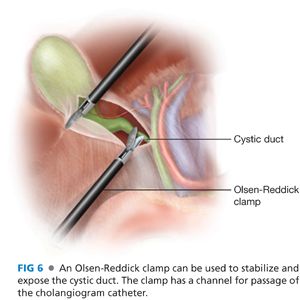
■ This method remove the use of clips along the cystic duct during IOC.
■ Infundibular approach
■ This approach is less technically demanding than direct cannulation of the cystic duct. It is also of value should identification of the cystic duct be difficult secondary to inflammation or scarring of the porta hepatis; however, in this clinical setting, the cystic duct may be occluded, precluding the approach.
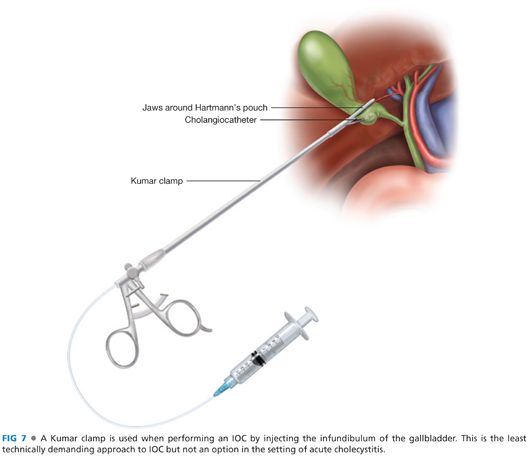
■ The peritoneum should be incised and the infundibulum dissected free from the hepatic bed. Once the infundibulum is mobilized, a Kumar clamp should be inserted through a laterally placed subcostal trocar. This clamp has long, atraumatic jaws, which completely occlude the infundibulum, and a side channel for the introduction of a needle-tipped cholangiocatheter. The clamp is applied along the lower body of the gallbladder, just above Hartmann’s pouch (FIG 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


