Intraductal Papillary Mucinous Neoplasm
Mari Mino-Kenudson, MD
Key Facts
Terminology
Grossly visible, mucin-producing epithelial neoplasm
Predominantly grows within main duct &/or its branches
Classified into main duct, combined, or branch duct type
Clinical Issues
Most frequent cystic tumor of pancreas
Symptoms associated with intermittent pancreatic ductal obstruction by tenacious mucin
Classic endoscopic finding: Mucin extravasation from patulous ampulla of Vater
Prognosis better than conventional ductal adenocarcinoma
Noninvasive tumors: 5-year survival rate > 75%
Invasive tumors: 5-year survival rate is 34-62%
Invasive components may be very focal, requiring submission of the entire lesion
Microscopic Pathology
Composed of mucin-secreting columnar epithelial cells with varying degrees of atypia
Classified as having low-grade dysplasia, moderate dysplasia, high-grade dysplasia, or invasive carcinoma arising in IPMN
4 epithelial subtypes
Gastric
Intestinal
Pancreatobiliary
Oncocytic
TERMINOLOGY
Abbreviations
Intraductal papillary mucinous neoplasm (IPMN)
Definitions
Grossly visible, mucin-producing epithelial neoplasm that primarily grows within main duct &/or its branches
Subclassification based on type of duct involvement
Main-duct type
Mucinous epithelium confined to main pancreatic duct
Combined type
Mucinous epithelium involving both main duct and branch ducts
Branch-duct type
Mucinous epithelium confined to branch ducts
CLINICAL ISSUES
Epidemiology
Incidence
Most common cystic tumor of pancreas
Approximately 8-20% of all resected pancreatectomy specimens
Age
Range: 25-94 years
Average: 63 years
Gender
Slightly more common in men
Presentation
Symptoms associated with intermittent pancreatic ductal obstruction
Abdominal pain
Back pain
Anorexia
Weight loss
Recurrent episodes of pancreatitis
Symptoms often present for months to years before diagnosis is established
Growing number of cases discovered incidentally during imaging for another indication
Endoscopic Findings
Mucin extravasation from patulous ampulla of Vater
Treatment
Surgical resection is treatment of choice
80-98% of IPMNs are surgically resectable
Prognosis
Noninvasive tumors: 5-year survival rate > 75%
Invasive tumors: 5-year survival rate is significantly lower (34-62%) than for noninvasive tumors
Still significantly better than that of conventional pancreatic ductal adenocarcinoma
IMAGE FINDINGS
CT Findings
Main-duct or combined type
Markedly dilated main duct often associated with dilated large branch ducts
Branch-duct type
Single or numerous cysts that represent dilated branch ducts
ERCP Findings
Dilated main pancreatic duct &/or branch ducts in absence of stricture
Filling defects due to papillary projections of neoplasm &/or mucous plugs
MRCP Findings
In addition to dilated ducts, mural nodules are better visualized
Indicative of higher grade lesion
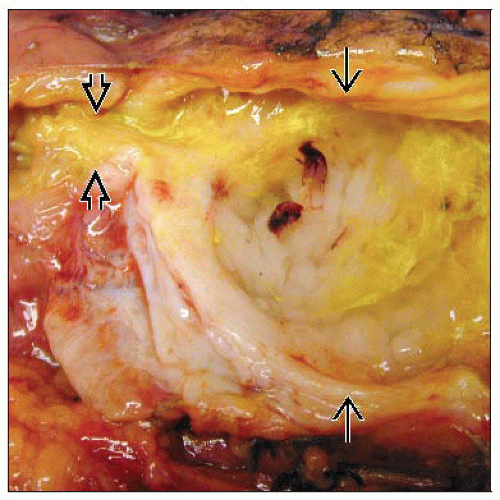
MACROSCOPIC FEATURES
General Features
Most common in pancreatic head
Often involve only a portion of pancreatic duct
Some are multifocal
Entire gland may be involved
Main-duct and combined types
Florid papillary projections, often in background of dilated ducts
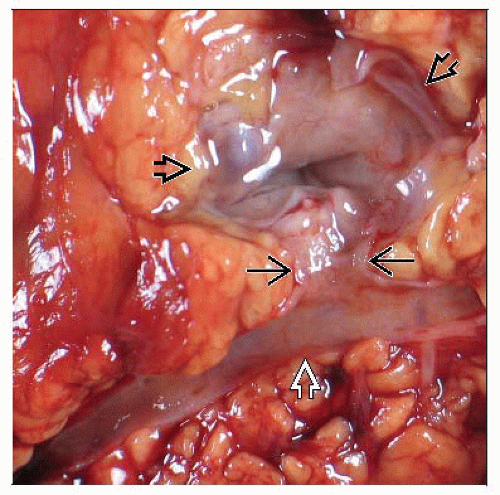
Branch-duct type
Single or multiple peripheral cysts that connect to main duct, often with smooth lining
Mural nodules &/or solid components may be seen in IPMNs with invasion
MICROSCOPIC PATHOLOGY
Histologic Features
Usually have papillary architecture
Do not have ovarian-type stroma
4 epithelial subtypes of mucin-secreting columnar epithelium
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree